This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Training the immune system to prevent cancer—researchers discover paradigm-shifting approach
As one of the most insidious diseases in the world, cancer has few treatments that work to eradicate it completely. Now, a new approach pioneered by two researchers working at the University of Missouri's Roy Blunt NextGen Precision Health building shows promising results in preventing lung cancer caused by a carcinogen in cigarettes—a discovery that immunologists Haval Shirwan and Esma Yolcu rank among the most significant of their careers.
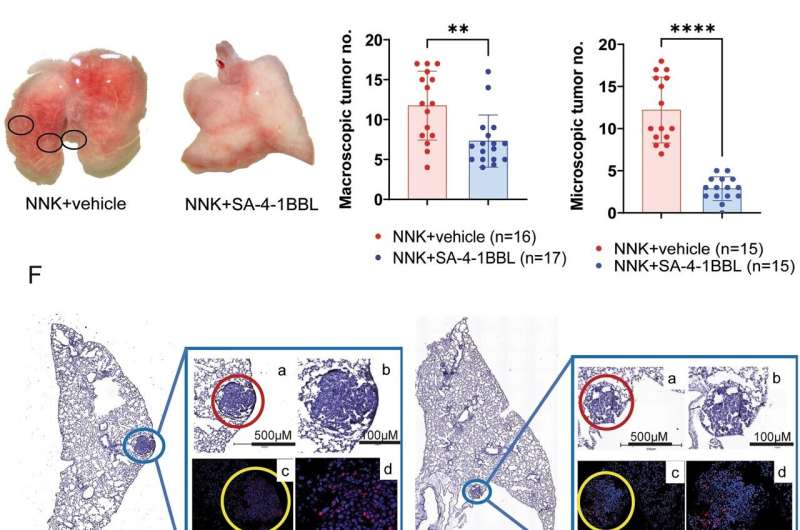
In the new study, Shirwan and Yolcu designed a molecule—known as an immune checkpoint stimulator (SA-4-1BBL)—that can mobilize immune cells and guide them along the pathway that most efficiently attacks cancer cells. The molecule not only reduces the number of nodules on cancerous tumors, but it also has the potential to prevent lung cancer by triggering and mobilizing the immune system to recognize and target cells in the body that could potentially become cancerous.
"This is huge," said Shirwan, a professor in the Department of Pediatrics and Molecular Microbiology and Immunology at the MU School of Medicine. "I have not been, over the entire course of my scientific career, as excited about a discovery as this one. When we started working with this molecule—a long time ago now—nobody thought the immune system had anything to do with cancer. Now, after years of immunotherapy advances, we know that's key to combating it."
Solving for solutions
The immune system works with checks and balances, said Yolcu, also a professor in the Department of Pediatrics and Department of Molecular Microbiology and Immunology at the MU School of Medicine.
"Two cells get together; one surveys the body for an unusual signal and presents it to another cell for interpretation, and the other cell receives it and generates an immune response if deemed critical for the survival of the host," she said.
Most immunotherapies are specific to certain cancer types and only have about a 15% to 30% efficacy. This new molecule, however, protects against several cancer types by teaching the immune system how to recognize when a body's cells are becoming cancer cells.
Shirwan likens the process to how an army works—where leaders equip soldiers with the appropriate weapons they'll need to go into combat successfully.
"This molecule can train the immune system to react to unknown factors, which in this case are cancer cells," Shirwan said.
The immune system is perceived to have evolved to fight against infections as external dangers and works in two stages: Its first response is rapid and proceeds through a process called innate immunity, which is not very sophisticated and modestly effective, that keeps bacteria and viruses at bay. Then, the immune system transitions into a more sophisticated, effective, and long-lasting adaptive immunity phase, which eliminates the pathogens and keeps them from coming back.
"Our data show that the immune system utilizes the same strategy against cancer as an internal danger. Preventing cancer, instead of treating it, is quite exciting from the efficacy as well as safety perspectives," said Shirwan.
It's now possible to screen high-risk individuals for the genes that can predict common cancers like breast and lung cancer, Yolcu said. This research could also help doctors develop a revolutionary approach for identifying groups who have a high risk of developing lung cancer—including people who are exposed to harmful smoke fumes—and be able to treat them proactively.
This breakthrough, SA-4-1BBL, patented in the U.S., Japan and the European Union, could also be used with various other immunotherapy treatments in the clinic.
"A novel agonist of 4-1BB costimulatory receptor shows therapeutic efficacy against a tobacco carcinogen-induced lung cancer" was published in Cancer Immunology, Immunotherapy.
More information: Ayse Ece Gulen et al, A novel agonist of 4-1BB costimulatory receptor shows therapeutic efficacy against a tobacco carcinogen-induced lung cancer, Cancer Immunology, Immunotherapy (2023). DOI: 10.1007/s00262-023-03507-2



















