This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Designing non-hallucinogenic psychedelic treatments that may accelerate research on mental health benefits
There is nothing magic about the recent increase in interest around the study of psychedelic drugs as potential treatments for patients suffering from a myriad of mental health conditions.
"The excitement follows the science," says John McCorvy, Ph.D., assistant professor of cell biology, neurobiology and anatomy at the Medical College of Wisconsin (MCW). "The number of landmark studies continues to grow, and the potential has caught the attention of academia and the pharmaceutical industry."
The legal status of psychedelic compounds slowed research progress to a crawl for decades before some studies began to garner regulatory approval in the early 2000s. Even in approved clinical trials, the hallucinogenic properties of these drugs lead to additional hurdles. Research participants need to take the substances under strict supervision in a clinical setting.
Trained therapists monitor participants for a long time as the length of a hallucinogenic experience ranges from about four to 12 hours depending on the drug and the individual. The treatment can cause confusion and anxiety for some patients who do not respond well to hallucinations, underscoring the need for vigilant health care personnel.
For those who have tolerated the drugs and associated hallucinations, however, promising studies have indicated that participants have experienced a substantial and sustained improvement in symptoms after taking a single dose.
"We've seen double-blind, placebo-controlled trials with psilocybin where patients with major depressive disorder reported improved symptoms for months," Dr. McCorvy says. "It is unheard of to get those kinds of results, especially without the patient having to take a pill every day." Psilocybin is a naturally occurring psychedelic compound made by hundreds of types of fungi, often referred to as "magic" mushrooms.
As promising as these and other results may be, however, the legal and practical hurdles for scientists and would-be research participants continue to loom large. But what if you could remove the hallucinogenic properties of possible psychedelic treatments without reducing their therapeutic potential?
MCW scientists published results in Nature Communications from experiments investigating what causes a psychedelic compound to elicit hallucinogenic experiences and how this characteristic can be manipulated by drug designers to create new psychedelic treatments for depression.
"There was no clear answer as to why a drug is hallucinogenic just based on chemical structure," Dr. McCorvy says.
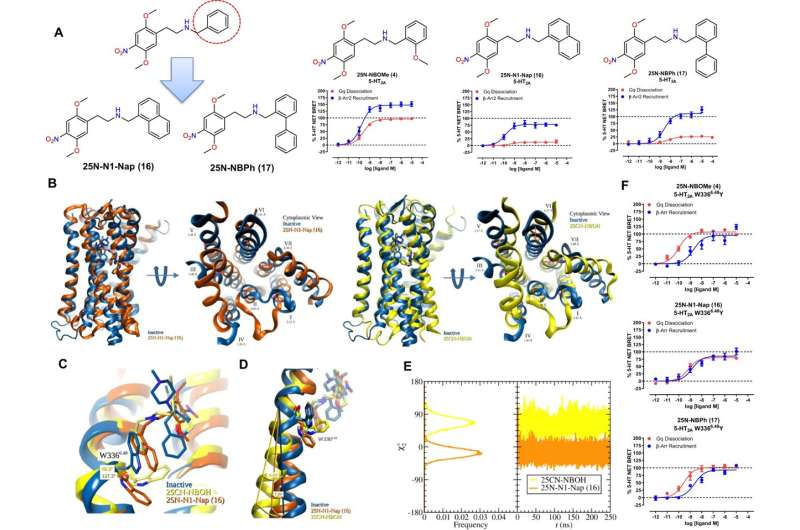
To better understand the source of hallucinogenic potential in these compounds, the scientists began by investigating a serotonin receptor called 5-HT2A that is found on the surface of cells throughout the central nervous system. It appeared likely to be involved in hallucinogenic potential based on other research findings.
The team knew that psilocybin and other well-known psychedelics would increase activity in this receptor, but it was unknown whether the compounds would favor one of two potential cellular signaling pathways. The scientists found that psychedelics did not completely favor either the Gq signaling pathway (the G protein responsible for typical cellular signaling) or the β-arrestin pathway (a protein that competes with Gq for the binding site to decrease signaling activity into the cell).
"We know that G protein signaling pathways are like the gas pedal for signaling and the β-arrestin pathway is like the brakes," Dr. McCorvy says. "Our question was, which of these signaling pathways is responsible for the hallucinogenic effects?"
To find out, scientists at St. Joseph's University, led by assistant professor Jason Wallach, Ph.D., synthesized hundreds of compounds and Dr. McCorvy's lab profiled their ability to selectively activate one of the two pathways through the serotonin 5-HT2A receptor.
Compounds that feature this type of pathway-selective activation are known as biased agonists. Ultimately, the team found the most effective option for discovering biased agonists is by adding additional molecular bulk to one of the compounds they had synthesized. This atomic manipulation reduced the Gq signaling while preserving the β-arrestin activity.
Then, Adam Halberstadt, Ph.D., and his lab at the University of California San Diego began testing the compounds in mice using an automated head twitch measurement that predicts psychedelic potential in humans. They found that these modified psychedelic biased agonist compounds with reduced Gq signaling did not induce a number of head twitches that correlates to hallucinogenic experiences, suggesting Gq signaling from the 5-HT2A receptor is necessary for psychedelic effects.
"We took a psychedelic and made it non-psychedelic, and we did it in a structure-based fashion," Dr. McCorvy says. "Hopefully in the future this will help increase study of these compounds if the hallucinogenic hurdles can be removed."
Dr. McCorvy would like to see industry build on this research by developing and testing new potential psychedelic treatments without the hallucinogenic trip.
"My vision is to get some of these compounds properly vetted in trials and out to clinics in my lifetime," Dr. McCorvy says. "I know too many people who have suffered from post-traumatic stress disorder and other mental health conditions without enough relief from current therapies. They need new treatment options as soon as it is prudent and possible."
More information: Identification of 5-HT2A Receptor Signaling Pathways Associated with Psychedelic Potential, Nature Communications (2023). DOI: 10.1038/s41467-023-44016-1




















