This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
proofread
Personalizing treatment for colorectal cancer patients by combining tissue-based biomarkers and ctDNA
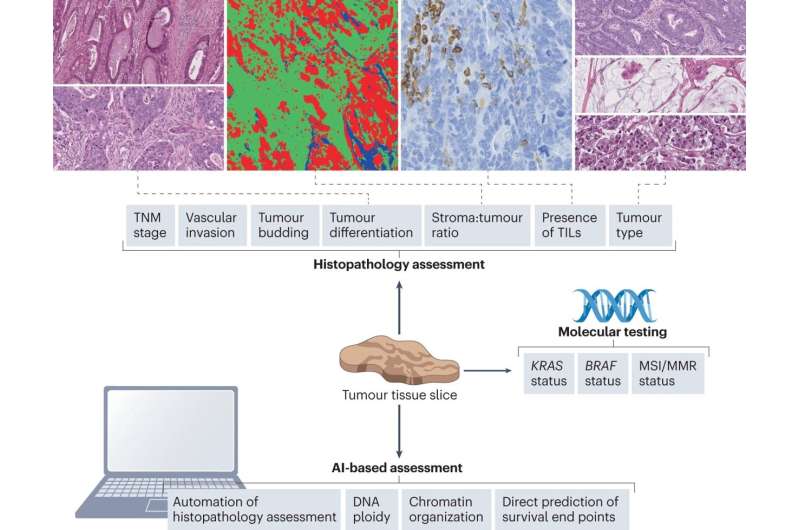
Combining artificial intelligence-generated digital pathology tools, conventional histopathological assessment and circulating tumor DNA (ctDNA) analysis can improve treatment stratification of patients with colorectal cancer after surgery. David Kerr and colleagues outline this novel paradigm for personalized adjuvant treatment of colorectal cancer in a study in Nature Reviews Clinical Oncology.
For patients with colorectal cancer (CRC), it is estimated that 80% of cancer recurrence occurs within three years after surgical resection. The selection of adjuvant therapy depends on conventional histopathological staging procedures, which constitutes a blunt tool for patient stratification.
The benefits of adjuvant therapy are relatively marginal and it is clear that there is a need for better methods for selecting patients who will benefit the most from the treatment while sparing those who will not derive benefit.
The better we understand the likelihood of cancer recurrence, the better we can tailor our adjuvant therapy, providing a more truly personalized treatment, emphasizes David Kerr, Professor at the University of Oxford and former president of the European Society for Medical Oncology (ESMO)
Liquid biopsies detecting ctDNA have been shown to have clinical utility for early detection of recurrence through surveillance and thus has the potential to personalize management of CRC patients. However, the analysis of ctDNA is costly, and the initial assessment of a patient's status usually occurs no earlier than four weeks following curative surgery and two weeks after completing systemic therapy.
This delay is due to the persistence of elevated levels of cell-free DNA for several weeks post-treatment. Given the uncertain consequences of delaying potential chemotherapy, and the fact that some patients may not show detectable ctDNA at their initial follow-up assessment, we propose using tissue-based biomarkers to facilitate an early pre-selection of treatment.
Improved patient management
Current clinicopathological markers are not good enough alone to accurately stratify patients with early-stage CRC. Three years ago, a study in The Lancet demonstrated how artificial intelligence (AI) can be used to predict CRC patient outcomes. The AI marker, named DoMore-v1-CRC, predicts the likelihood of cancer-specific death directly from images of routine histopathology sections.
Building on these findings, the marker has since then been integrated with established clinicopathological markers to provide a clinical decision support system (CDSS) for guiding the choice of adjuvant chemotherapy in stage II and III CRC without residual disease after surgery.
Compared to conventional risk stratification for adjuvant therapy, the proposed CDSS identifies a much larger group of patients with an excellent prognosis that are likely to have similar survival with and without adjuvant chemotherapy and can therefore be spared the severe side effects of the treatment.
Since the CDSS's recommendation can be determined within a few days after surgery, patients identified as high-risk can begin treatment soon after surgery. In addition, the CDSS would identify additional strong candidates for adjuvant chemotherapy among those that are ctDNA negative at first assessment. Patients classified as low risk by the CDSS would then enter a ctDNA monitoring program and receive treatment upon ctDNA detection, if any.
"I believe that integrating tissue and blood-borne prognostic biomarkers, as we suggest in this article, does make sense in regard to a more personalized treatment," says Professor Kerr. "With this combined approach, adjuvant treatment can be spared for more than half the patients with high-risk stage II and III CRC. These patients are very unlikely to benefit from the adjuvant treatment.
"This novel paradigm will reduce the economic cost and personnel requirements as well as improve the management of patients by more truly personalized treatment, which is ultimately the goal."
More information: Li Yang et al, Personalizing adjuvant therapy for patients with colorectal cancer, Nature Reviews Clinical Oncology (2023). DOI: 10.1038/s41571-023-00834-2

















