This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Researchers treat consequences of brain injuries with nasally administered stem cell secreted factors
Brain injuries cause widespread damage to brain tissue. Damaged cells begin to produce signaling molecules that trigger processes of inflammation, apoptosis—programmed cell death—and oxidative stress. After the acute phase (about a day), chronic neuroinflammation occurs. It can last a long time and cause secondary damage with negative consequences, including behavioral and cognitive dysfunction.
RUDN University doctors have shown that glial cells help mitigate neuroinflammation due to brain injuries. More precisely, it is the small "bubbles" they produce—vesicles—which carry proteins and other compounds.
"Glial cells release a wide range of physiologically active substances in extracellular vesicles to support neurons. We investigated whether it is possible to use extracellular vesicles of glial cells to protect neurons in a model of traumatic brain injury," Diana Salikhova, Ph.D., Head of the Laboratory of Cellular Biotechnology of RUDN University said.
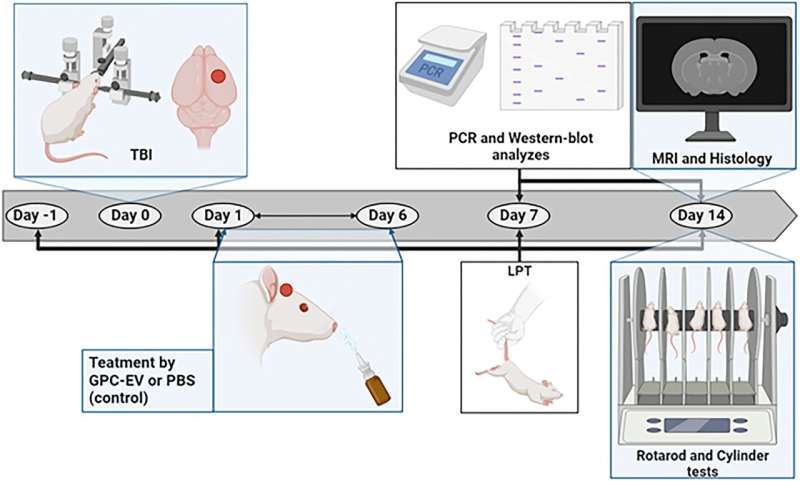
Doctors experimented on 30 adult rats. The animals were surgically subjected to an artificial brain injury, after which 15 animals were intranasally injected with extracellular vesicles of glial cells after the injury. The glial cells themselves were obtained from induced pluripotent stem cells from healthy donors. A week later, RUDN doctors checked the condition of the animals' brain tissue using PCR analysis and Western blotting. After another week, the authors conducted a series of tests to determine the behavioral characteristics of the animals.
The damaged area in animals receiving vesicles decreased slightly—by only 4 cubic millimeters. However, the therapy contributed to a significantly faster recovery of the animals' brain functions, improving the sensorimotor functions of the damaged hemisphere and reducing inflammation. For example, the number of CD68+ macrophages responsible for inflammation decreased threefold after therapy.
The level of the caspase enzyme, which triggers apoptosis, decreased by 2.5 times. RUDN University doctors also discovered a molecular mechanism that explains this effect. Supposedly, 203 types of small non-coding nucleotide sequences, microRNAs, became agents of neuroprotective action.
"Extracellular vesicles from glial cells have shown therapeutic effects in traumatic brain injury. They stimulated nervous system recovery and neuroplasticity. In addition, we found 203 types of microRNAs, which apparently can be used to treat various brain pathologies," Diana Salikhova, Ph.D., Head of the Laboratory of Cellular Biotechnology of RUDN University said.
More information: Diana I. Salikhova et al, Extracellular vesicles of human glial cells exert neuroprotective effects via brain miRNA modulation in a rat model of traumatic brain injury, Scientific Reports (2023). DOI: 10.1038/s41598-023-47627-2


















