This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Liver fibrosis scores as predictors of long-term outcomes in patients with ST-segment elevation myocardial infarction
Liver fibrosis scores (LFSs) are novel tools for predicting cardiovascular events in patients with coronary artery disease. A study appearing in Cardiovascular Innovations and Applications aimed at examining the prognostic value of LFSs in patients with ST-segment elevation myocardial infarction (STEMI).
Between 2015 and 2019, 866 patients diagnosed with STEMI were consecutively enrolled. The definition of major cardiovascular events (MACEs) was all-cause death, nonfatal myocardial infarction, nonfatal ischemic stroke, and acute limb ischemia.
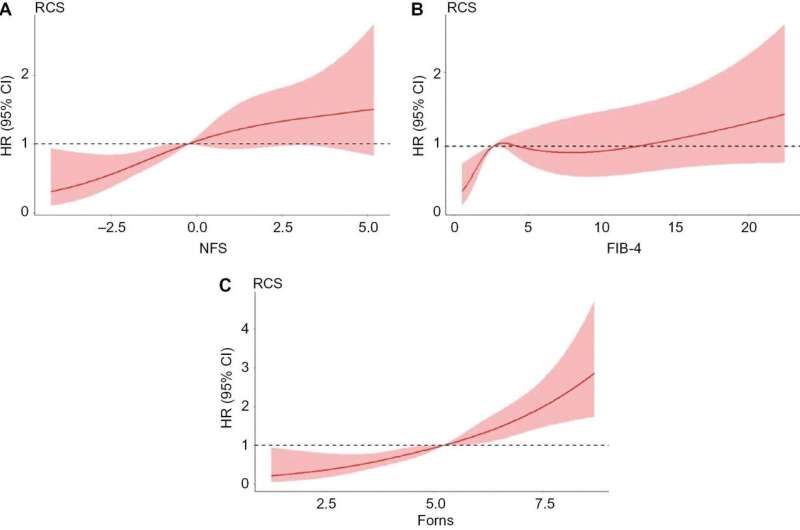
The authors evaluated the predictive values of LFSs for MACEs with receiver operating characteristic (ROC) curve and restricted cubic spline (RCS) analysis. Kaplan-Meier (K-M) analysis was conducted to explore the relationship between LFSs and MACEs.
During a median follow-up of four years, 155 MACEs were observed. K-M analysis of MACEs revealed significantly lower event-free survival rates in patients with intermediate or high, rather than low, NFS, FIB-4, BARD, and Forns scores.
The multivariable-adjusted hazard ratios (95% CI) for MACEs in patients with high versus low risk scores were 1.343 (0.822–2.197) for NFS, 1.922 (1.085–3.405) for FIB-4, 2.395 (1.115–5.142) for BARD, and 2.271 (1.250–4.125) for Forns.
The ROC curve indicated that the predictive ability for MACEs was non significantly improved by addition of the NFS (AUC = 0.7274), FIB-4 (AUC = 0.7199), BARD (AUC = 0.7235), and Forns (AUC = 0.7376) scores into the basic model (AUC = 0.7181). RCS revealed a tendency toward a nonlinear positive association of MACEs with NFS, FIB-4, and particularly Forns scores.
LFSs have potential utility for predicting adverse outcomes in patients with STEMI, thus indicating the importance of managing metabolic dysregulation.
More information: Longyang Zhu et al, Liver Fibrosis Scores as Predictors of Long-term Outcomes in Patients with ST-segment Elevation Myocardial Infarction, Cardiovascular Innovations and Applications (2024). DOI: 10.15212/CVIA.2023.0095





















