This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Blood test could reveal cause of brain injury in newborn babies
Researchers from Imperial College London have shown that a blood test can pinpoint the underlying cause of brain injury in newborns.
Their study looked at babies with a type of brain injury caused by hypoxia—a lack of oxygen. It found that patterns of gene expression that are detectable in the blood can point to the cause of the injury and tell doctors if the newborn is likely to respond to cooling treatment, commonly used to treat brain injury in infants.
The findings, published in the journal JAMA Network Open, could eventually lead to a simple test to quickly diagnose brain injury in newborns and help with treatment decisions.
The study included babies from low and middle-income countries (LMICs) as well as high-income countries (HICs). There was a dramatic divergence in gene expression between the two groups suggesting a different underlying cause of brain injury.
Lead investigator, Professor Sudhin Thayyil from the Department of Brain Sciences at Imperial College London, explains, "Although cases of brain injury in babies may appear similar, they can be quite different in terms of how they come about, as our study shows. The gene expression patterns we saw in babies from LMICs were similar to what you would see in people with sleep apnea, suggesting that they experienced intermittent hypoxia in the womb and at birth.
"We believe this is brought on by multiple chronic stresses during pregnancy such as poor nutrition or infection, as well as the normal labor process and uterine contractions, which leads to further hypoxia and ultimately injury to the baby's brain.
"On the other hand, gene expression patterns in babies from HICs suggested a single, acute cause of brain injury, for example complications during birth like maternal bleeding, leading to a sudden drop in blood oxygen levels in the fetus."
A driver of newborn mortality
Hypoxic-ischemic encephalopathy (HIE) is a type of brain injury sometimes referred to as birth asphyxia, which occurs when a baby's brain does not get enough oxygen before or shortly after birth.
Globally, HIE is a leading cause of death and disability among babies born at full term, affecting about 3 million babies every year. Following oxygen deprivation, brain injury can develop over hours to months and affect different regions of the brain, resulting in a variety of potential neurodisabilities such as cerebral palsy, epilepsy, deafness or blindness.
South Asia, and particularly India, has the highest disease burden, with the country accounting for 60% of all HIE-related deaths in the world.
Previous studies, mainly conducted in high-income countries (HICs), have shown that treatment with whole-body cooling can improve outcomes for babies with HIE. As result, it has become standard practice in many HICs, and is also used in some hospitals in South Asia.
However, in the largest study of its kind in low- and middle-income countries (LMICs), Professor Thayyil and collaborators in India, Bangladesh and Sri Lanka previously showed that whole-body cooling actually worsened outcomes in babies with HIE and might have even increased mortality risk.
The new study helps to explain the reason behind this difference in treatment response between the two groups of babies and could eventually lead to a simple test to evaluate which babies are likely to benefit from cooling treatment.
Comparing gene expression
The study, led by Imperial and its South Asian partners, included 35 babies born with HIE in Italy (a HIC), and 99 babies from LMICs in South Asia (India, Sri Lanka and Bangladesh). Blood samples were taken shortly after birth and the babies were medically assessed at 18 months of age.
In total, about half the babies in the South Asian cohort died or developed severe disabilities, compared to a quarter in the Italian cohort.
The researchers looked for correlations between gene expression at birth and outcomes at 18 months in both cohorts. They found 1,793 significant genes associated with adverse outcome in the HIC cohort and 99 significant genes associated with adverse outcome in the South Asian cohort. There were only 11 significant genes in common between the cohorts—but they were expressed in opposite directions (either switched on in one cohort and off in the other, or vice versa).
Study co-author Professor Swati Manerkar, from Lokmanya Tilak Municipal Medical College in Mumbai, India, comments, "We were expecting to see some differences in gene expression between babies in the cohorts—but not such a dramatic divergence. It clearly shows that we are seeing are very different causes of brain injury between the two groups, with different characteristics which also helps to explain why some babies respond to cooling and others are harmed by it."
Guiding treatment decisions
The researchers stress that the differences between the cohorts are not related to ethnicity, but rather socioeconomic factors. The type of chronic brain injury commonly seen in LMICs is also likely to be present in deprived areas in HICs. Likewise, among more affluent populations in LMICs, one would expect to see more cases of acute brain injury of the type mostly seen in HICs in the present study.
Professor Thayyil comments, "The key for clinicians, anywhere in the world, is to be able to identify which type of brain injury they are dealing with as soon as possible—and that's something we're currently working on."
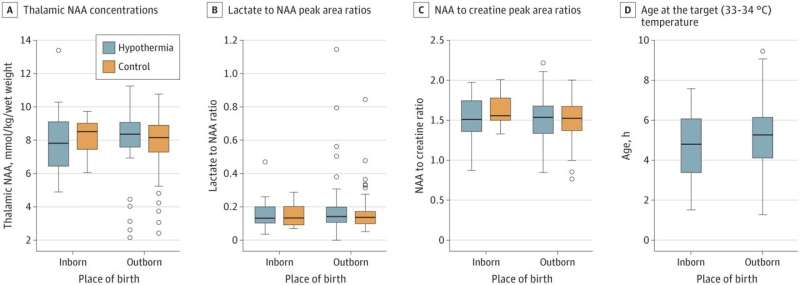
More information: Sudhin Thayyil et al, Whole-Body Hypothermia, Cerebral Magnetic Resonance Biomarkers, and Outcomes in Neonates With Moderate or Severe Hypoxic-Ischemic Encephalopathy Born at Tertiary Care Centers vs Other Facilities, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.12152


















