This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Study explores characteristics associated with poor COVID-19 antibody response
Adults with certain socio-demographic and clinical characteristics may have weaker antibody responses to COVID-19 vaccination, which could leader to a higher risk of infection, according to a recent study published in Nature Communications.
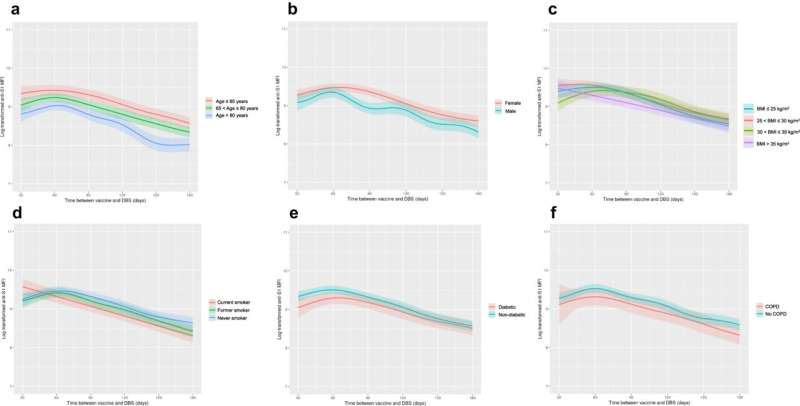
The study found that U.S. adults with lower antibody levels after COVID-19 vaccination were 65 years or older, male, had a higher body mass index, smoked or had a history of smoking, had a history of diabetes or chronic obstructive pulmonary disease, and who had received the Pfizer (BNT162b2) COVID-19 vaccine.
The findings emphasize that these patient groups may need to receive more frequent COVID-19 booster vaccinations to prevent future infections, according to Norrina Allen, Ph.D., MPH, the Quentin D. Young Professor of Health Policy, director of the Center for Epidemiology and Population Health and a co-author of the study.
"It means that these individuals who are losing their antibody response faster after vaccination and may be at a higher risk for COVID infection. They probably need more frequent boosters to make sure that they're protected from future COVID infections," said Allen, who is also a professor of Preventive Medicine in the Division of Epidemiology, Medical Social Sciences and of Pediatrics.
According to the World Health Organization, more than 700 million people have been diagnosed with COVID-19 since March 2020. Of those cases, more than 100 million Americans have been diagnosed with the disease, and is currently one of the leading causes of death in the U.S.
The development of messenger RNA (mRNA) vaccines drastically reduced COVID-19 infections and severe illness. The vaccines help the body produce anti-S1 (IgG) antibodies against the spike protein of SARS-CoV-2, the virus that causes COVID-19, and the amount of antibodies present determines how likely a patient's body can fight off COVID-19 infection.
In the current study, which was conducted as part of the National Institutes of Health Collaborative Cohort of Cohorts for COVID-19 Research (C4R) program, the investigators investigated characteristics that were associated with anti-S1 antibody response following COVID-19 vaccination in more than 6,000 American adults.
The average age of participants was 73 years; 58% of participants were female and 76% were white. Additionally, 52% of participants received the Pfizer (BNT162b2) COVID-19 vaccine and 48% received the Moderna (mRNA-1273) COVID-19 vaccine.
Participants' anti-S1 antibody levels were measured from dried blood spots collected by participants between February 2021 and August 2022 by using an at-home finger-pricking method.
Overall, lower anti-S1 antibody levels following COVID-19 vaccination were associated with participants who were 65 years or older, male, had a higher body mass index, who smoked or had a history of smoking, had a history of diabetes or chronic obstructive pulmonary disease, and who received the Pfizer COVD-19 vaccine.
"Everyone's antibody rates decline over time, but for some people these declines happen earlier and faster putting them at greater risk for COVID infection. This is important because those are the same groups that we see the highest risk for severe COVID hospitalization and poor outcomes from COVID," Allen said.
Participants who had prior COVID-19 infection and were hospitalized also demonstrated higher anti-S1 antibody levels, according to the study.
Allen noted that a limitation of the study was it didn't investigate the correlation between COVID-19 infection rates and anti-SI antibody levels, but that it will be studied going forward.
"We don't fully know the relationship between antibody levels and future COVID risk particularly for PASC, which is essentially long-COVID, but that's the next step," Allen said.
According to Allen, the current findings should be considered by health care providers who may need to encourage patients in these groups to get more frequent COVID-19 booster vaccinations and to work with public health officials to establish more personalized vaccination recommendations for these patients.
"We should think about the person as an individual and make our booster recommendations based on that as opposed to this kind of one-size-fits-all approach," Allen said.
More information: John S. Kim et al, Demographic and Clinical Factors Associated With SARS-CoV-2 Spike 1 Antibody Response Among Vaccinated US Adults: the C4R Study, Nature Communications (2024). DOI: 10.1038/s41467-024-45468-9



















