This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Micro-massaging—'artificial muscles' help fractured leg bones heal better
Orthopedic implants are used to fixate the bone fragments of fractures. Novel smart implants are now being developed that can continuously monitor and actively promote bone healing—by, for example, micro-massaging the fracture site. This innovative medical technology is currently under development at Saarland University by an interdisciplinary team of medical specialists, engineers, and computer scientists.
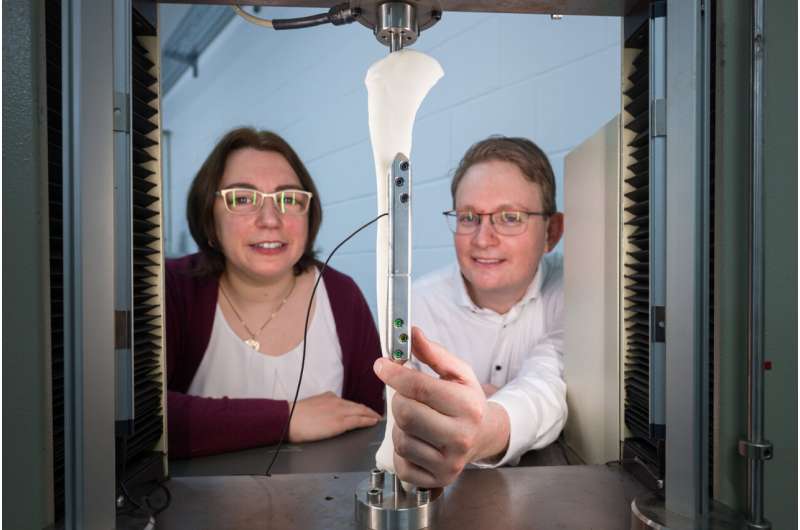
The team of engineers led by Professors Stefan Seelecke and Paul Motzki has equipped the implant with smart 'artificial muscles'. Fabricated from shape memory wires, these 'muscles' provide a way to control the fracture repair process via smartphone. The team will be exhibiting their prototype at this year's Hannover Messe.
Bones are both stable and elastic; they grow, they are constantly renewing themselves and they are built to withstand a lot of force. If a bone breaks, it can heal, provided that the fragments are properly aligned. But sometimes, things don't work out as planned, and despite being operated on, the fracture doesn't heal as it should. This is particularly common in patients who have suffered a fracture of the lower leg—affecting around fourteen in every hundred cases.
Once the leg has been operated on, the physician treating the patient can't simply look inside the leg to see how the bone repair process is progressing. It is only weeks later, when the first X-ray image is taken that doctors can see whether new bone tissue is growing as it should. When that is not the case, the result is typically pain, incapacity to work, and high costs.
However, a new type of orthopedic implant is now offering a way to monitor the fracture repair process continuously and even actively encourage the bone to heal. This innovative medical technology is being developed by a large interdisciplinary team of medical specialists, engineers, and computer scientists at Saarland University.
"We're developing a smart implant that does not require any additional surgical intervention or additional equipment. An orthopedic implant is typically a passive fixation plate that is used to set and stabilize the fractured bone. But we can now give it completely new capabilities," explained Professor Stefan Seelecke, who heads research groups at Saarland University and at the Center for Mechatronics and Automation Technology (ZeMA).
As soon as the fixation plate has been attached and the wound sutured, the implant begins providing a continuous stream of information on how the fracture is healing. If the patient puts too much pressure on the fracture, the smart implant will give a warning.
At the fracture gap, where the bone fragments have been realigned with each other, the implant can be made locally more or less rigid as required; it can even undergo tiny motions to deliver a 'micro-massage' to the fracture site. This kind of 'micro-manipulation' at the surface of the bone actively promotes healing by stimulating growth. And these processes can all be fully automated using a smartphone.
The smart implants have been developed on the basis of expert input from a range of specialist fields.
Nickel-titanium 'shape memory' wires no thicker than human hair play a central role in these advanced orthopedic implants. The engineering side of the project is managed by the two Saarbrücken professors, Stefan Seelecke and Paul Motzki, who are experts in intelligent materials systems.
"We use these shape memory wires as mechanical actuators that can alter the local rigidity of the implant and can make it move or exert a force. But we also use them as sensors to monitor processes taking place at the fracture site," explained Paul Motzki, who holds a cross-institutional professorship in smart material systems for innovative production at Saarland University and at ZeMA.
The ultrafine nickel-titanium wires can contract or relax like real muscle fibers, depending on whether an electric current is flowing or not. The reason for this behavior lies in the crystal structure of the alloy. "Nickel-titanium alloy is what is known as a shape memory material. At the level of the crystal lattice, the alloy can exist in two phases that can transform into each other," explained Paul Motzki.
"If electric current flows through the wire, the material heats up, causing it to adopt a different crystal structure with the result that the wire becomes shorter. When the current is switched off, the wire cools down and returns to its original length. The engineers fabricate bundles of these fine wires, just as muscle fibers in nature are grouped into fiber bundles. By alternately tensing and relaxing the wires, the engineers can simulate the movement of flexor or extensor muscles.
"The more wires we have, the greater the surface area and the faster we can dissipate heat, which means faster contractions," said Stefan Seelecke. The wires are able to exert a substantial force over a very short distance. "These wires have the highest energy density of all known drive mechanisms, and they can deliver a substantial tensile force," explained Seelecke further.
But these artificial muscles also have their own intrinsic sensor properties. "When the wires change shape, so too does their electrical resistance. We can assign precise resistance values to even the smallest of deformations, which allows us to extract sensory data," said Susanne-Marie Kirsch, who is doing doctoral research in the Saarbrücken group.
The measurement data enable the team to monitor minute changes occurring in the gap between the bone fragments. The engineering team collaborates closely with the overall project leads at Saarland University: trauma surgeon Professor Tim Pohlemann and Professor of Innovative Implant Development Bergita Ganse.
This close monitoring of the fracture gap enables the medical team to assess whether fracture site stiffness increases over time. In the future, this sensor data will be transmitted wirelessly to a smartphone. Close interdisciplinary collaboration between the project sub-teams allows conclusions to be drawn about how targeted mechanical stimulation of the fracture site can best be used to promote bone healing.
By careful data modeling and programming, the researchers are able to choreograph highly precise motion sequences for the fixation plate to perform.
At this year's Hannover Messe, the research team will be demonstrating a prototype smart orthopedic implant that makes use of artificial muscle fibers. These electrically responsive fibers can be positioned above the fracture site. Electrical signals can then be applied to control whether the artificial muscle fibers elongate, contract, or remain unchanged, thus determining the local rigidity of the fixation plate at the fracture site.
The researchers can control the artificial muscles that span the fracture gap so that they expand and contract at the required frequency. A stroke amplitude in the range of 100–500 micrometers produces the best results. Thanks to their intrinsic sensor properties, these bundles of shape memory wires also effectively serve as the implant's nervous system.
If it becomes harder to contract the artificial muscles positioned across the fracture gap, this is a good indication that the bone tissue in this region is becoming harder, and the healing process is progressing. A semiconductor chip controls the system.
"The control unit is able to precisely correlate the electrical resistance data with the extent of deformation of the wires so that bone healing can be stimulated by carefully controlled movements of the plate, effectively micro-massaging the fracture site," explained Ph.D. student Felix Welsch, who is also helping to develop the smart implant.
Once in place, the implants can be left to do their work. Even charging is carried out remotely: "The implant will be fitted with a powerful battery that can be recharged in situ via wireless induction," said Paul Motzki.




















