This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Peripheral artery system at risk of disease due to family history, lifestyle
Most people have heard of heart attacks occurring because of a blocked coronary artery. But the body has two types of artery systems: the coronary artery system, which relates to the heart, and peripheral artery system, which involves the arteries carrying oxygenated blood to the arms, legs, brain and the rest of the body.
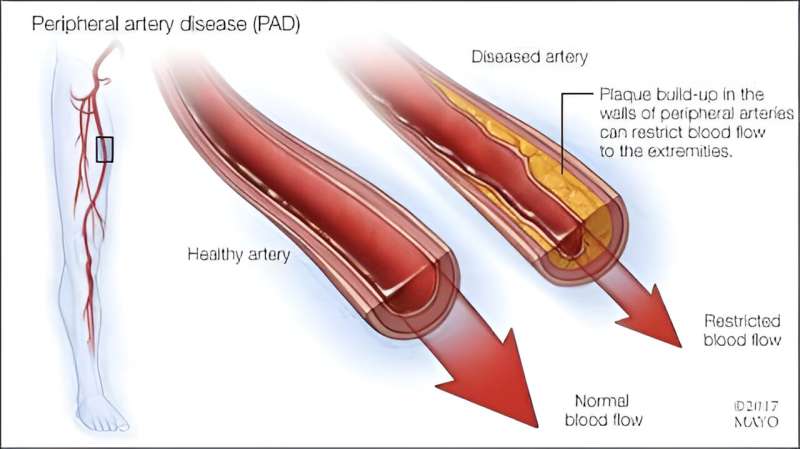
"Just like coronary arteries, peripheral arteries can become diseased," says Michel Barsoum, M.B., Ch.B., a cardiologist and vascular medicine specialist at Mayo Clinic Health System in Chippewa Falls, Eau Claire and Rice Lake, Wisconsin. "This condition, called peripheral artery disease, or PAD, narrows arteries and reduces blood flow due to a buildup of fatty and calcium deposits on the artery walls."
This can cause claudication, which is muscle pain and cramping when a person is active but usually disappears after a few minutes of rest.
Risk factors for peripheral artery disease
"So who is at risk of peripheral artery disease? People who smoke or have diabetes at any age are at the greatest risk," says Dr. Barsoum.
Other risk factors include:
- Body mass index over 30.
- Family history of PAD, heart disease or stroke.
- High blood pressure.
- High cholesterol.
- Increasing age, especially if you are 65 or older.
Symptoms include:
- Aching or cramping in the arms when knitting, writing or performing other manual tasks.
- Change in the color of your leg or arm.
- Coldness of the lower leg or foot even after walking in a warm weather.
- Sores on the toes, feet or leg that don't heal.
- Weakening pulse in the foot.
- Erectile dysfunction in men.
- Hair loss on the legs.
"If neck arteries to your brain are affected, symptoms may include difficulty talking, weakness in the arms and legs, or loss of vision," says Dr. Barsoum. "If you experience any of these symptoms, make an appointment with a vascular medicine specialist, who will conduct a physical exam and record your health history."
The exam will include finding a pulse in the affected neck artery and comparing it with the pulse in the unaffected neck artery. Vascular medicine specialists have a wide range of tools available, depending on the degree of your symptoms, to help you return to the activities you love.
For example, if you can walk a few blocks with only mild pain, they may prescribe medications such as aspirin, statins or blood thinners. They also may discuss ways you can modify your risk factors, including quitting smoking; controlling blood pressure, cholesterol and diabetes; and increasing your activity level.
If you have more significant symptoms, such as not being able to tolerate the pain when walking, a vascular medicine specialist typically will order an ultrasound or a CT scan with contrast, or even an angiogram to determine the location and degree of the blockage. Your care team will discuss a variety of surgical options to deal with the blockage.
"Prevention of peripheral artery disease is always the best treatment," says Dr. Barsoum. "Quit smoking, eat a heart-healthy diet, exercise regularly, keep your blood sugar in check if you have diabetes, maintain a healthy weight, and manage your blood pressure and cholesterol levels."
In addition, if you have one or more risk factors, avoid certain over-the-counter cold remedies that contain pseudoephedrine. These medications constrict your blood vessels and might worsen your symptoms.




















