This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Researchers identify new genetic risk factors for persistent HPV infections
Human papillomavirus (HPV) is the second most common cancer-causing virus, accounting for 690,000 cervical and other cancers each year worldwide. While the immune system usually clears HPV infections, those that persist can lead to cancer, and a new finding suggests that certain women may have a genetic susceptibility for persistent or frequent HPV infections.
These genetic variants, identified in a study led by University of Maryland School of Medicine researchers, could raise a woman's risk of getting cervical cancer from a high-risk HPV infection.
Findings were recently published in the European Journal of Human Genetics.
The research team conducted a genome-wide association study of high-risk HPV infections in a cohort of over 10,000 women, whose data were collected as part of the African Collaborative Center for Microbiome and Genomics Research (ACCME) cohort study.
A total of 903 of the participants had high-risk HPV infections when the study began, with 224 participants having HPV infections that resolved and 679 having persistent HPV infections. More than 9,800 HPV-negative women from the ACCME study served as controls.
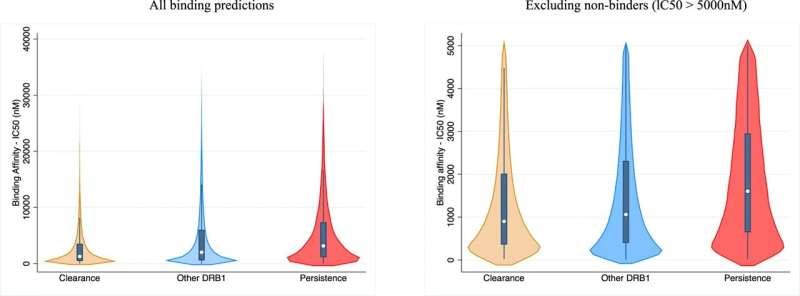
"We found certain genetic variants were associated with having high-risk HPV infections, while other variants and human leukocyte antigen (HLA) genes were associated with persistent infections, which increase the risk of developing cervical cancer," said study leader Sally N. Adebamowo, MBBS, MSc, ScD, Associate Professor of Epidemiology & Public Health at UMSOM.
"This is a critical finding that suggests genetic underpinnings for cervical cancer risk. It is the first sufficiently powered genome-wide association study of cervical high-risk HPV infections. Our polygenic risk score models should be evaluated in other populations."
Specifically, she and her colleagues found that the top variant associated with prevalent high-risk HPV infection was rs116471799, on the fourth chromosome near the LDB2 gene, which encodes proteins. They found persistent HPV was associated with variants clustered around the TPTE2, a protein-encoding gene associated with gallbladder cancer.
The genes SMAD2 and CDH12 were also associated with persistent high-risk HPV infections and significant polygenic risk scores. Together, the findings enabled the research team to develop polygenic risk scores to determine the likelihood that a certain genetic profile would increase the risk of having prevalent or persistent HPV infections.
"Our findings can be used to stratify persistent high-risk HPV infections for precision or personalized cervical cancer prevention. We hope to conduct long-term studies on the integration of PRS and genomic risk factors into the continuum of cervical cancer prevention," said study corresponding author Clement A. Adebamowo, BM, ChB, ScD, Professor of Epidemiology & Public Health at UMSOM.
A recent report from the American Cancer Society found that cervical cancer among women ages 30 to 44 rose almost 2 percent a year from 2012 to 2019. This is after a big decline in cervical cancer rates over the past half-century due to early detection from Pap smears and HPV screening tests. In addition, rates of cervical cancer have steadily declined among younger women, who were among the first to benefit from HPV vaccines, which were approved for use in 2006.
In the U.S., more than half of women diagnosed with cervical cancer have never been screened or were not screened in the last five years, according to the Centers for Disease Control and Prevention. In Nigeria, only a small percentage of women have access to the HPV vaccine, so those included in the study were largely unvaccinated.
"The results provide insight into the role of antigen processing and presentation and HLA-DRB1 alleles in immune surveillance and persistence of high-risk HPV infections," said Mark T. Gladwin, MD, who is the John Z. and Akiko K. Bowers Distinguished Professor and Dean, UMSOM, and Vice President for Medical Affairs, University of Maryland, Baltimore.
"Confirmatory studies are crucial to validate these important findings in other populations, with the goal of reducing the burden of high-risk HPV-related diseases on global health."
More information: Sally N. Adebamowo et al, Genome, HLA and polygenic risk score analyses for prevalent and persistent cervical human papillomavirus (HPV) infections, European Journal of Human Genetics (2024). DOI: 10.1038/s41431-023-01521-7




















