This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Liver lesions at risk of transformation into hepatocellular carcinoma in cirrhotic patients: Study
Hepatocellular carcinoma (HCC) represents a significant global health burden as one of the most common malignancies in individuals with chronic liver disease or cirrhosis. This malignancy evolves through a multistep process, beginning with dysplastic nodules (DNs) and early HCC, progressing to overt HCC.
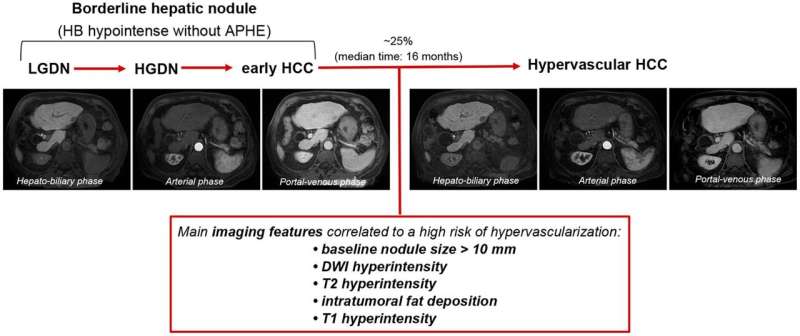
Recent advancements in liver imaging, particularly the use of hepatocyte-specific contrast agents, have enhanced the detection of these precursor lesions, known as borderline hepatic nodules. These nodules, especially those hypointense in the hepatobiliary phase (HBP) without arterial phase hyperenhancement (APHE), present a diagnostic challenge and a significant risk of malignant transformation.
The use of liver-specific contrast agents, such as gadoxetic acid, in magnetic resonance imaging (MRI) has revolutionized the detection and characterization of hepatic nodules. In the HBP, these agents highlight the lack of functioning hepatocytes in malignant or pre-malignant nodules, which appear hypointense against the background of normal liver parenchyma. This imaging technique has improved the diagnostic accuracy for small HCC lesions (
Moreover, the integration of diffusion-weighted imaging (DWI) with gadoxetic acid-enhanced MRI has further increased the specificity and sensitivity in identifying HCC, even for nodules smaller than 1 cm. This combination helps distinguish true HCC from benign hypervascular pseudolesions, which is crucial for appropriate clinical management.
Borderline hepatic nodules encompass a spectrum of lesions, including DNs and early HCCs. Pathologically, these nodules exhibit varying degrees of cytological and architectural atypia. High-grade dysplastic nodules (HGDNs) and early HCCs often display unpaired arteries and intermediate sinusoidal capillarization, but lack significant vascular invasion, making them difficult to distinguish from low-grade dysplastic nodules (LGDNs) on imaging alone.
The expression of organic anion-transporting polypeptide 8 (OATP8) is notably reduced in these nodules, leading to their characteristic hypointensity in the HBP on MRI. This reduction in OATP8 expression occurs early in hepatocarcinogenesis, prior to the development of the vascular changes typical of overt HCC.
The detection of HBP hypointense nodules without APHE has significant clinical implications. Studies have shown that the initial size of these nodules is a strong predictor of malignant transformation. Nodules larger than 10 mm at initial detection have a higher risk of progression to hypervascular HCC. This risk necessitates a vigilant and tailored follow-up strategy for patients with such nodules.
However, there is a lack of consensus on the management of these nodules. The variability in study populations and follow-up periods has led to inconsistent findings regarding the risk factors and natural history of these lesions. Some studies suggest that antiviral therapies, such as direct-acting antivirals (DAAs) for hepatitis C, may reduce the rate of hypervascular transformation, although this remains a topic of ongoing research.
In conclusion, the detection and management of borderline hepatic nodules, particularly those hypointense in the HBP without APHE, are critical in preventing the progression to overt HCC. Advances in imaging technologies, specifically the use of liver-specific contrast agents and DWI, have significantly improved our ability to detect and characterize these nodules.
Understanding the pathological features and natural history of these lesions is essential for developing standardized guidelines for their management. Further research is needed to refine these strategies and optimize patient outcomes.
This review highlights the current state of knowledge regarding borderline hepatic nodules, emphasizing the importance of early detection and individualized patient management to mitigate the risk of HCC development. The findings are published in the Journal of Clinical and Translational Hepatology.
More information: Nicolò Brandi et al, Liver Lesions at Risk of Transformation into Hepatocellular Carcinoma in Cirrhotic Patients: Hepatobiliary Phase Hypointense Nodules without Arterial Phase Hyperenhancement, Journal of Clinical and Translational Hepatology (2023). DOI: 10.14218/JCTH.2023.00130





















