This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Study shows weak associations between psychiatric symptoms and selected inflammatory biomarkers
A new study published in Psychoneuroendocrinology shows weak associations between psychiatric symptoms and selected inflammatory biomarkers in patients with chronic pain. The study found that sickness behavior contributed more to explaining psychiatric comorbidity.
"The patients in this study had several symptoms, but the associations with the investigated inflammatory biomarkers were weak or non-existent. Despite high levels of self-reported sickness behavior, the inflammatory level was generally within the normal range.
"Interestingly, sickness behavior was more important in explaining depression and insomnia than inflammatory markers," says the study's first author, Jenny Åström Reitan, at the Department of Clinical Neuroscience, Karolinska Institutet.
More data on the associations between psychiatric comorbidity, sickness behavior, and inflammatory markers may improve understanding of important mechanisms in chronic pain.
Understanding more about experienced sickness, as measured by sickness behavior, can help improve treatments for these symptoms and be a possible target for treatment. The results show the complexity of chronic pain and the difficulty in identifying biomarkers.
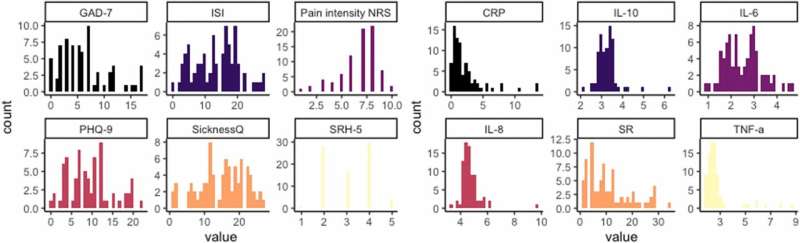
Self-reported questionnaires and blood samples to analyze levels of inflammatory biomarkers were collected from 80 adult patients with chronic pain at Karolinska University Hospital. The associations between inflammatory biomarkers (TNF-α, IL-6, IL-8, IL-10, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR)) and depression, insomnia, anxiety, self-rated health, sickness behavior, and pain intensity were analyzed.
The next step is to investigate the relationship between pain interference, inflammatory biomarkers and sickness behavior.
More information: Jenny L.M. Åström Reitan et al, Associations between sickness behavior, but not inflammatory cytokines, and psychiatric comorbidity in chronic pain, Psychoneuroendocrinology (2024). DOI: 10.1016/j.psyneuen.2024.107094





















