This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Factors influencing extravasation of newborn intravenous infusions
Newborns, particularly premature infants, are highly vulnerable during intravenous infusion treatments due to their low immunity, inability to express discomfort, and fragile veins.
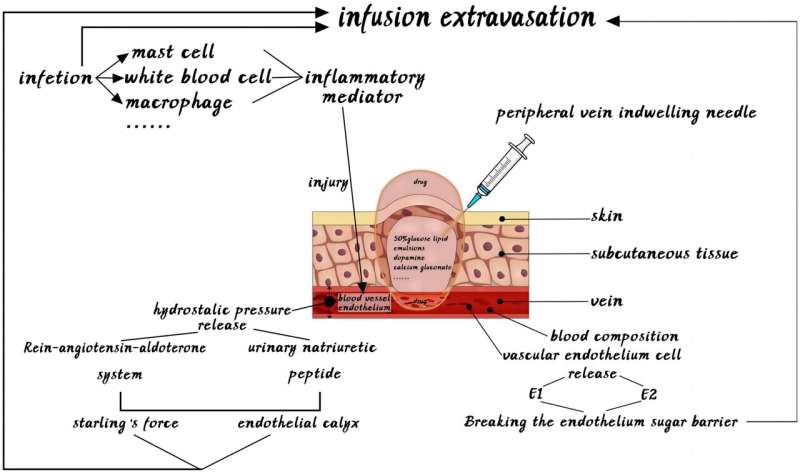
Extravasation, the leakage of infusion fluids into surrounding tissues, is a significant concern that can lead to severe complications, including tissue necrosis, infection, and even death. This essay reviews the intrinsic and extrinsic factors contributing to neonatal infusion extravasation, emphasizing the importance of early detection and intervention to prevent severe outcomes. The research is published in the journal Exploratory Research and Hypothesis in Medicine.
Chemical stimulation of blood vessels due to intravenous drugs is a primary factor causing extravasation. Drugs with high osmotic pressure, such as 50% glucose and lipid emulsions, can lead to dehydration and necrosis of tissue cells, causing sterile inflammation.
Vasoactive drugs like dopamine, adrenaline, and noradrenaline cause peripheral blood vessel constriction, leading to tissue ischemia and increased vascular permeability, which heightens the risk of extravasation. Furthermore, drugs like calcium gluconate, used to prevent metabolic bone disease in neonates, can cause lysosomal rupture, autolysis, and inflammatory changes, leading to tissue damage and necrosis.
The infusion rate and temperature significantly affect the likelihood of extravasation. Rapid infusion rates can overwhelm local blood vessel capacity, causing phlebitis and extravasation. Long-term infusion of irritant solutions should be avoided, with continuous infusions limited to less than two hours.
Additionally, maintaining an appropriate infusion temperature is crucial, as excessively low temperatures can cause local blood vessel spasms and increase vascular permeability, thereby raising the risk of extravasation.
The type of infusion tools and the chosen site for infusion also influence the risk of extravasation. Peripheral intravenous catheters are preferred over disposable steel needles, as they cause less irritation to blood vessels and can remain in place for 3–4 days, reducing the need for repeated punctures.
However, the risk of extravasation increases with prolonged catheter placement. Infants and young children are more prone to extravasation in the lower limbs than the upper limbs, and important veins are more sensitive to irritating drugs, increasing the likelihood of venous inflammation and extravasation.
The proficiency of nurses in using peripheral intravenous catheters, their knowledge of intravenous infusion, and their clinical experience are critical in preventing extravasation. Inexperienced nurses may struggle with vein selection and control of puncture depth, leading to repeated punctures and mechanical damage to blood vessels.
Factors such as a weak sense of responsibility, inadequate inspection of infusion sites, and insufficient inspection frequency can further contribute to extravasation risks. Emotional stability and psychological qualities of nurses, influenced by environmental factors like instrument alarms and infant crying, also play a significant role in the success rate of punctures.
Certain neonatal diseases can increase the likelihood of intravenous fluid extravasation. Conditions such as acute respiratory distress syndrome, meconium aspiration pneumonia, neonatal asphyxia, and pulmonary hypertension can cause lesions in blood vessels or subcutaneous tissues, enhancing the risk of extravasation. These diseases involve inflammatory processes, changes in vascular permeability, and structural defects in skin proteins, all of which can contribute to the extravasation of intravenous fluids.
Understanding the various factors influencing neonatal infusion extravasation is crucial for developing effective prevention and intervention strategies. By addressing chemical stimulation, infusion rates, temperature management, appropriate selection of infusion tools and sites, and improving nurse training and disease management, health care providers can significantly reduce the incidence of extravasation and improve outcomes for neonates undergoing intravenous therapy.
More information: Fang Huang et al, Factors Influencing Extravasation of Newborn Intravenous Infusions: A Review, Exploratory Research and Hypothesis in Medicine (2023). DOI: 10.14218/ERHM.2023.00030



















