This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Research team explores etiologies of splenic venous hypertension
Splenic venous hypertension (SVH), also known as left-sided portal hypertension, is a rare condition characterized by upper gastrointestinal (GI) bleeding in the absence of liver disease. This condition arises due to increased pressure in the splenic vein (SV), causing blood to drain through the short gastric veins to the stomach, leading to the dilation of submucosal structures and the formation of gastric varices. Unlike traditional portal venous hypertension (PVH), SVH does not involve elevated pressures in the main portal vein and is primarily an extrahepatic condition.
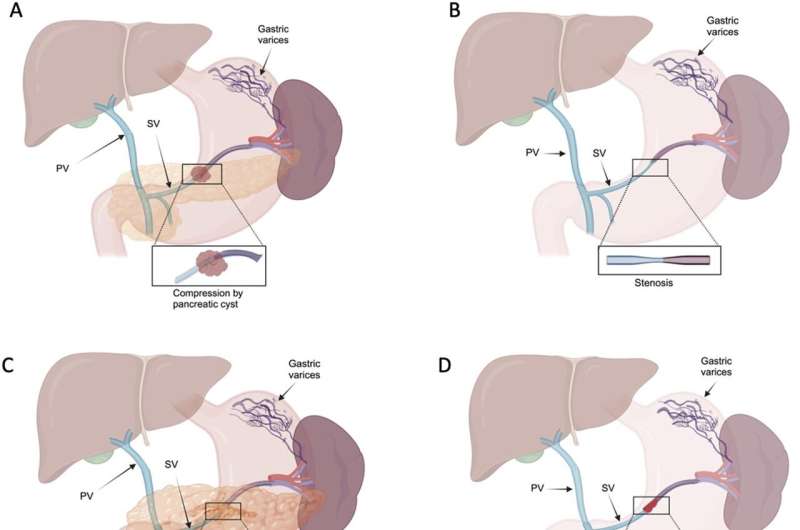
Diagnosing SVH requires a high degree of clinical suspicion, especially in patients presenting with upper GI variceal bleeding, splenomegaly, and normal liver enzyme tests. SVH can develop through various mechanisms, including compression, stenosis, inflammation, thrombosis, and surgically decreased splenic venous flow.
A new review in the Journal of Clinical and Translational Hepatology explores this condition.
Compression of the splenic vein is a significant cause of SVH, accounting for approximately 18% of cases. This can occur due to external compression by neighboring structures such as benign neoplasms, adenocarcinoma, non-functioning neuroendocrine tumors (NETs), anatomical variants, and Bochdalek hernia. These structures exert pressure on the splenic vein, obstructing blood flow and increasing venous pressure, leading to gastric varices.
Stenosis of the splenic vein is a rare cause of SVH. Idiopathic splenic vein stenosis can lead to increased venous blood flow in the gastric veins, resulting in varices. It is characterized by the narrowing of the splenic vein with post-stenotic dilatation and the absence of other common causes such as pancreatitis, pancreatic tumors, cysts, thrombosis, or arterial aneurysms.
Inflammatory conditions such as pancreatitis can lead to fibrosis and subsequent occlusion of the splenic vein, increasing venous pressure and causing gastric varices. Studies have shown that splenic vein obstruction due to inflammation is more frequent in males, with a median age of 48. Severe cases of acute pancreatitis (AP) have a higher incidence of SVH compared to mild cases.
Thrombosis of the splenic vein can occur due to conditions such as essential thrombocythemia (ET) and primary myelofibrosis (PMF). This leads to increased blood flow in the gastric veins, forming varices. Splenic vein thrombosis is a serious condition that requires prompt diagnosis and management to prevent complications.
Surgical interventions for pancreatic cancer, such as pancreatoduodenectomy (PD) and portal-superior mesenteric vein (PV-SMV) resection, can lead to decreased venous flow in the splenic vein. This results in vascular congestion, increased pressure within the venous system, and the formation of gastric varices. This complication is more common in the late stages of PD, as increased survival time due to surgery provides a greater length of time for the development and bleeding of varices.
Patients with SVH typically present with symptoms of upper GI bleeding, which often occurs due to ruptured gastric varices. Splenomegaly and normal liver function tests are common clinical findings. Asymptomatic presentations are also frequent, with many cases being identified incidentally. In symptomatic cases, abdominal pain and hypersplenism with thrombocytopenia and pancytopenia are common. Unlike portal hypertension caused by liver disease, ascites is uncommon in SVH due to the absence of underlying liver cirrhosis.
Diagnosis of SVH involves a combination of clinical suspicion and imaging studies. The typical presentation includes GI bleeding with gastric varices, splenomegaly, and normal liver function tests. Initial imaging usually involves transabdominal ultrasound (US) with Doppler, although this has limited efficacy for visualizing the SV. More detailed imaging, such as contrast-enhanced endoscopic ultrasound (EUS), computed tomography angiography (CTA), or magnetic resonance angiography (MRA), is often required to assess the patency and anatomy of the splenic vasculature. Endoscopic methods, such as esophagogastroduodenoscopy (EGD), are crucial for identifying and managing varices.
The management of SVH is primarily focused on addressing the underlying cause of splenic venous obstruction and managing variceal bleeding. Treatment options vary depending on the etiology.
Surgical and endoscopic approaches
For cases where the SV obstruction is due to tumors or anatomical anomalies, surgical interventions such as splenectomy or distal pancreatectomy may be necessary. Endoscopic interventions, such as band ligation or variceal injection, are critical for controlling acute bleeding episodes.
Splenic artery embolization
This less invasive procedure is often preferred in patients who are not candidates for splenectomy due to previous complex abdominal surgeries. It reduces splenic venous pressure and helps control variceal bleeding.
Pharmacological treatments
Beta-blockers and octreotide are used to manage portal hypertension and prevent recurrent variceal bleeding. Lifelong anticoagulation therapy is recommended for patients with thrombosis-related SVH, particularly those with conditions such as factor V Leiden or paroxysmal nocturnal hemoglobinuria (PNH).
The prognosis of patients with SVH largely depends on the underlying cause. Patients with pancreatic cancer generally have poorer outcomes due to the aggressive nature of the disease and shorter life expectancy. For non-malignant causes, proper management of the underlying condition typically leads to a favorable prognosis. GI bleeding, although a severe complication, is relatively rare, and with appropriate management, the risk of fatality can be minimized.
In conclusion, SVH is a rare but significant condition that requires a high index of suspicion for diagnosis, particularly in patients presenting with variceal bleeding and splenomegaly without liver disease. The condition arises due to increased pressure in the SV from various causes, leading to variceal formation and bleeding. Effective management hinges on addressing the underlying cause and controlling bleeding.
While surgical interventions like splenectomy remain a cornerstone of treatment, less invasive approaches such as splenic artery embolization and pharmacological management are becoming increasingly important. Continued research is needed to improve diagnostic modalities and develop less invasive treatment options.
More information: Jasmine Tidwell et al, Etiologies of Splenic Venous Hypertension: A Review, Journal of Clinical and Translational Hepatology (2024). DOI: 10.14218/JCTH.2024.00054




















