This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Unexplainable chronic itch shows unique blood biomarkers that could eventually lead to new targeted treatments
Millions of patients worldwide suffer from a chronic itching condition with no identifiable cause—a condition known as chronic pruritus of unknown origin (CPUO)—that has no targeted therapies approved to treat it. Many of these patients suffer for years with little relief, but a new University of Maryland School of Medicine study may provide hope for future treatments. Patients were found to have lower than normal levels of metabolite biomarkers in the blood plasma that could point to a cause of their excruciating symptoms.
Findings were recently published in the journal Scientific Reports.
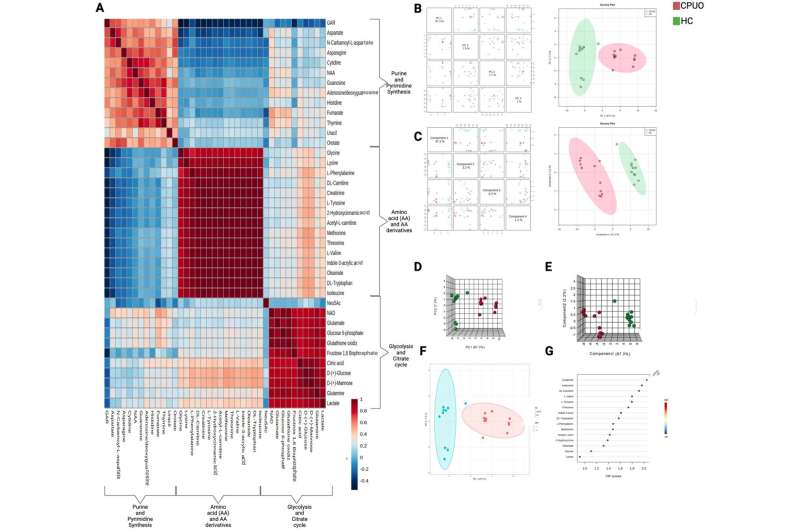
"Our study found a distinct deficit in certain metabolite biomarkers, including several important amino acids and other metabolites involved in immune system regulation in patients with CPUO compared to a healthy control group," said study principal investigator Shawn Kwatra, MD, the Joseph W. Burnett Endowed Professor and Chair of Dermatology at UMSOM and Chief of Service Dermatology at the University of Maryland Medical Center (UMMC). "This is an exciting finding because it provides novel insights into the cause of this condition and identifies potential future therapeutic targets to consider."
Chronic pruritus of unknown origin is most prevalent among older adults and causes severe itching lasting longer than six weeks. Current therapies used to help manage symptoms are off-label and have poor efficacy, with many patients having a significantly impaired quality of life.
In the latest study, Dr. Kwatra and his colleagues compared blood plasma samples from patients with CPUO and matched healthy control patients. They found lower levels of nine amino acids in the CPUO patients compared to the control group and that the lower levels correlated with itch severity.
Previous animal studies have correlated low levels of these amino acids with itch symptoms in mice. These amino acids serve as building blocks for neurotransmitters, or brain chemicals, that play a role in the body's itch response and other allergic skin reactions. Providing mice with medications like antidepressants to boost neurotransmitters like serotonin was found to reduce itch symptoms.
"Many of these biomarkers that we found in depleted amounts in the blood of CPUO patients, like tryptophan and glycine, could contribute to the underlying pathogenesis of this condition, but we certainly need larger studies to investigate this further," said Dr. Kwatra.
Study co-authors also included faculty from Johns Hopkins University School of Medicine and Duke University Medical Center.
In June, Dr. Kwatra published a study in JAMA Dermatology showing that a drug targeting inflammation (abrocitinib), which is approved to treat eczema, provided significant improvement in itching symptoms in those with CPUO as well as another itching disorder called prurigo nodularis.
He also led a study, published last year in the New England Journal of Medicine, demonstrating the efficacy of the monoclonal antibody, nemolizumab, in treating prurigo nodularis. The drug was approved on August 13 by the US Food and Drug Administration and is one of the first FDA-approved treatments for this skin condition, which disproportionately affects African-American patients.
Dr. Kwatra is a consultant/advisor to several pharmaceutical companies, including the manufacturers of abrocitinib and nemolizumab. Since beginning his position at UMSOM earlier this year, Dr. Kwatra has created the Maryland Itch Center at the University of Maryland Medical Center.
More information: Jaya Manjunath et al, Plasma metabolomic profiling reveals a novel circulating biomarker signature in chronic pruritus of unknown origin, Scientific Reports (2024). DOI: 10.1038/s41598-024-67170-y


















