This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Investigational mpox mRNA vaccine more effectively reduces disease severity in primates compared to available vaccines
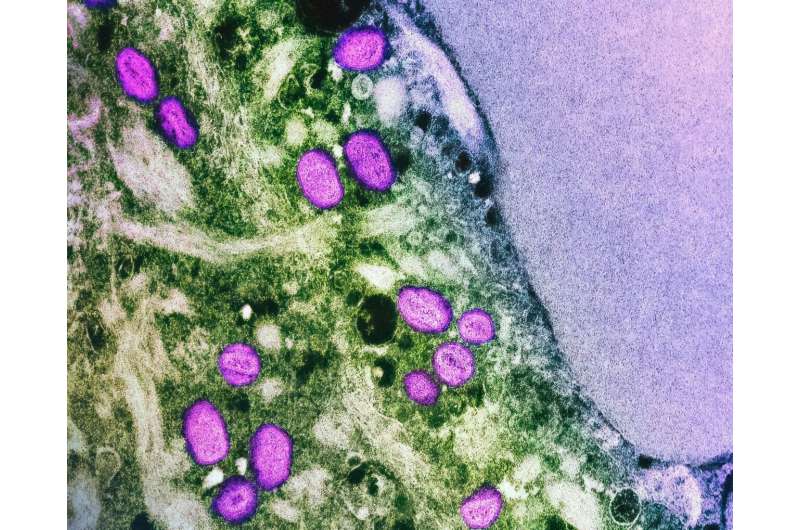
The most frequently used mpox vaccine provides partial immunity to the disease but isn't always able to prevent severe symptoms or disease transmission. A new vaccine candidate from Moderna, mRNA-1769, more effectively limits symptoms and disease duration in primates that were infected with a lethal strain of the mpox virus when compared to a currently licensed modified vaccinia Ankara (MVA) vaccine. The study was published September 4 in the journal Cell.
"This study is the first in a nonhuman primate model where we compare an investigational mRNA mpox vaccine directly to the current standard of care," says co-first author Alec Freyn, a virology researcher at Moderna.
"When we put those vaccines head-to-head in primates, we saw improved responses from the mRNA vaccine in terms of not just protection from survival but also fewer lesions, shorter duration of disease, and less viral shedding in the blood and respiratory tract."
MVA vaccines, which were originally developed to combat smallpox, contain whole viruses that have been weakened so that they cannot cause disease in humans. However, this weakening also means that they provide limited protection compared to other vaccines such as the potent but potentially infectious ACAM2000.
In comparison, using mRNA technology enables vaccines to be designed to include only the parts of the virus that are most likely to induce a lasting, protective immune response without exposing the person to a whole infectious virus. In this case, the investigational mpox mRNA vaccine is composed of four viral antigens that are critical for the virus to attach and enter host cells.
"With the mRNA vaccine, we're able to pick pieces of the virus that can give the most potent and most effective immune response," says senior author Galit Alter, virologist and immunologist at Moderna. "By doing that instead of being distracted by an entire virus, you're able to narrow down on the pieces of the virus that give you protection."
Though previous studies have shown that mRNA vaccines can prevent lethal mpox infections in nonhuman primates, their ability to limit disease severity hasn't previously been tested.
To directly compare the investigational mRNA vaccine to MVA vaccines, the researchers vaccinated six macaques with each vaccine and then exposed them to a lethal strain of mpox virus eight weeks after their initial vaccine dose. They also exposed a control group of six unvaccinated animals to the virus.
Following infection, the researchers monitored the animals' health for four weeks and collected blood samples to examine their immune response.
All 12 vaccinated animals survived the challenge, regardless of which vaccine was used, whereas five of six unvaccinated control animals succumbed to the disease.
Though both vaccines reduced disease severity compared to the control group, mRNA-vaccinated animals lost less weight and had fewer lesions than MVA-vaccinated animals—on average, animals in the control group had a maximum of 1,448 lesions, MVA-immunized animals had a maximum of 607 lesions, and mRNA-immunized animals had a maximum of 54 lesions.
The mRNA vaccine also shortened disease duration (the number of days for which the animals showed lesions) by more than 10 days compared to the MVA vaccine and resulted in lower viral loads in both blood and throat swabs, suggesting that it might also be more effective at reducing transmission.
"With the mRNA technology, we're able to produce a vaccine that gives quite potent responses with a very tolerable safety profile," says senior author and virologist Jay Hooper of the United States Army Medical Research Institute for Infectious Diseases.
"We've been trying to get a vaccine that will prevent spread like ACAM2000 but without the safety issues. This is showing that mRNA technology might be able to fill that niche."
When the researchers compared the immune response triggered by the mRNA and MVA vaccines, they found that the mRNA vaccine resulted in higher numbers of antibodies, as well as antibodies with more diverse immune functions. The team was able to identify different classes of antibodies that were associated with enhanced viral control and fewer lesions.
The mRNA vaccine also showed potential to induce cross-immunity to other Orthopoxviruses, whereas the MVA vaccine results in smaller immune responses that are not as strongly neutralizing for more remotely related Orthopoxviruses.
"We tested serum from the monkeys immunized with this vaccine against basically every Orthopoxvirus we could get our hands on," says Freyn. "It neutralized not only mpox but also vaccinia, cowpox, rabbitpox, camelpox, and ectromelia virus. We believe that this vaccine may protect from other Orthopoxvirus threats that may emerge in the future."
Moderna's mRNA-1769 vaccine is currently being assessed in a Phase I/II clinical trial (NCT05995275) to determine the safety, tolerability, and immune response of a range of doses of mRNA-1769.
More information: Comparison of protection against Mpox following mRNA-1769 or MVA vaccination in NHPs, Cell (2024). DOI: 10.1016/j.cell.2024.08.043





















