A step forward for stem cell therapy
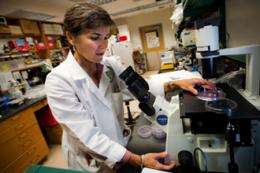
(Medical Xpress) -- A new study shows the potential of a method to prepare stem cells that may provide relief from a painful diabetes complication. Aline Betancourt of the Tulane University Center for Stem Cell Research and Regenerative Medicine, with colleagues at Tulane and the Ochsner Clinic Foundation, developed a new treatment using modified stem cells to control inflammation.
The study results released on Monday (July 9) in the journal Stem Cells Translational Medicine suggest that the use of stem cells specially prepared to turn off the body’s inflammatory response represent a promising new therapeutic strategy for diabetic peripheral neuropathy that should be further investigated.
About 70 percent of diabetics have neuropathy (nerve damage) resulting from the disease, according to the National Institutes of Health. Severe peripheral neuropathy causes excruciating pain in the toes, feet, legs, hands or arms. Even a tiny amount of external pressure can be excruciating. Inflammation is considered a major culprit.
Previous studies have proven mesenchymal stem cells (MSCs) are safe and effective in treating inflammatory diseases. MSCs, which are taken from adult donors, can give rise to a large number of tissue types such as bone, fat and cartilage.
“The problem,” Betancourt explains, “is that the current methods for preparing these cells yield a mixed pool of undefined cells that aren’t consistently effective in the clinic. Our laboratory developed a new method that results in a consistent, uniform MSC population and optimizes their anti-inflammatory effects. We call these cells MSC2s.”
When the researchers tested the MSC2 cells on mice with peripheral neuropathy, they saw a significant improvement in inflammation and other symptoms — as much as 40 percent for the MSC2 group over the mice that received no treatment. At best, there was only 14 percent improvement in those administered conventional MSCs.














