Researchers use iPSCs to define optimal treatment for managing life-threatening arrhythmias
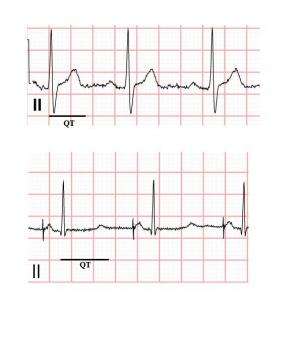
Researchers used induced pluripotent stem cells (iPSCs) derived from a young patient with Long QT syndrome (LQTS), a congenital heart disorder, to determine a course of treatment that helped manage the patient's life-threatening arrhythmias. The results, which appear in The Journal of General Physiology, could lead to improved treatments for LQTS and other channelopathies, diseases caused by disturbed ion channel function.
iPSCs—adult cells that have been genetically reprogrammed to function like embryonic stem cells—provide a valuable tool for studying diseases and developing customized drug therapies. Researchers from Columbia University Medical Center used iPSCs differentiated into cardiomyocytes (iPSCs-CMs) to study the physiological basis for arrhythmias in a four-year-old with LQTS.
The disease, which can cause arrhythmias that lead to seizures and sudden death, is caused by a mutation in any of various genes encoding cardiac ion channels or their associated proteins. In the case at hand, the child had mutation in the SCN5A gene, which encodes a sodium channel, and a common polymorphism in the KCNH2 gene, which encodes a potassium channel.
Using voltage clamp analyses of iPSCs-CMs derived from the affected child and his parents, the researchers determined that his arrhythmias were caused by the SCN5A mutation. They performed further in vitro testing using the iPSCs-CMs to identify the most appropriate regimen for correcting the aberrant activity associated with the defective ion channel.
The results show promise for using in vitro iPSC techniques in the development of individualized drug therapies for patients with LQTS and other channelopathies.
More information: Terrenoire, C., et al. 2013. J. Gen. Physiol. 141:61-72.



















