August 30, 2013 report
Vaccination may make flu worse if exposed to a second strain
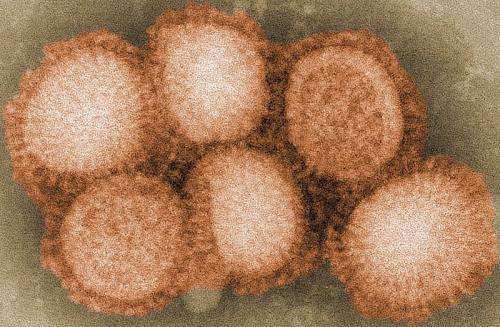
(Medical Xpress)—A new study in the U.S. has shown that pigs vaccinated against one strain of influenza were worse off if subsequently infected by a related strain of the virus.
Microbiologist Dr. Hana Golding of the Center for Biologics Evaluation and Research at Bethesda in Maryland and colleagues at the National Animal Disease Center in Ames, Iowa and elsewhere, vaccinated "naive" piglets (those that had never been exposed to flu viruses) against the H1N2 influenza strain and later exposed them to the rare H1N1 virus, which is the virus responsible for the 2009 swine flu pandemic.
When the piglets were vaccinated they produced a wide range of antibodies to block the H1N2 virus, but these "cross-reactive" antibodies not only failed to provide protection against the second virus, H1N1, but appeared to actually help the H1N1 virus infiltrate lung tissue and cause more severe symptoms and respiratory system complications such as pneumonia and lung damage. The unvaccinated controls suffered milder pneumonia and fewer other complications. This effect is called Vaccine-Associated Enhanced Respiratory Disease.
The researchers found that the antibodies produced in response to H1N2 could not bind to a key region of the H1N1 virus and could therefore neither kill nor neutralize them and stop them binding to cells in the pigs' lungs, and in fact helped the new virus to fuse to lung cells and multiply more readily, through a process the scientists dubbed "fusion enhancing."
The team concluded that this effect should be taken into consideration by researchers trying to develop a universal influenza vaccine to protect humans from all strains of flu virus, (see this article, for example) since protection against one strain may produce antibodies that assist similar, related strains of virus. They also cautioned that their results may not apply to humans, and that the vaccines they used were made from whole, killed viruses, unlike those used to protect humans, which are made from parts of killed viruses.
The current findings add weight to studies of the 2009 outbreak of H1N1 flu in Canada, which discovered that people who had received the normal seasonal flu vaccine were more likely to be affected by H1N1 than those who had not been vaccinated.
Dr Golding said the findings of their research are not relevant to regular seasonal flu vaccinations, and that she thought "people should definitely take them," but she added that the results of the research could prove useful for improving future vaccines.
The paper was published in the journal Science Translational Medicine on August 28.
More information: Vaccine-Induced Anti-HA2 Antibodies Promote Virus Fusion and Enhance Influenza Virus Respiratory Disease, Sci Transl Med 28 August 2013: Vol. 5, Issue 200, p. 200ra114 Sci. Transl. Med. DOI: 10.1126/scitranslmed.3006366
Abstract
Vaccine-induced disease enhancement has been described in connection with several viral vaccines in animal models and in humans. We investigated a swine model to evaluate mismatched influenza vaccine-associated enhanced respiratory disease (VAERD) after pH1N1 infection. Vaccinating pigs with whole inactivated H1N2 (human-like) virus vaccine (WIV-H1N2) resulted in enhanced pneumonia and disease after pH1N1 infection. WIV-H1N2 immune sera contained high titers of cross-reactive anti-pH1N1 hemagglutinin (HA) antibodies that bound exclusively to the HA2 domain but not to the HA1 globular head. No hemagglutination inhibition titers against pH1N1 (challenge virus) were measured. Epitope mapping using phage display library identified the immunodominant epitope recognized by WIV-H1N2 immune sera as amino acids 32 to 77 of pH1N1-HA2 domain, close to the fusion peptide. These cross-reactive anti-HA2 antibodies enhanced pH1N1 infection of Madin-Darby canine kidney cells by promoting virus membrane fusion activity. The enhanced fusion activity correlated with lung pathology in pigs. This study suggests a role for fusion-enhancing anti-HA2 antibodies in VAERD, in the absence of receptor-blocking virus-neutralizing antibodies. These findings should be considered during the evaluation of universal influenza vaccines designed to elicit HA2 stem-targeting antibodies.
© 2013 Medical Xpress
















