Hitting inflammation in the guts
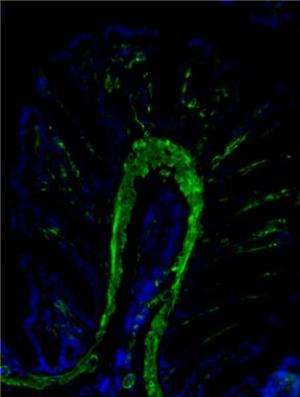
Researchers in UCD Conway Institute and Systems Biology Ireland have identified a way that a new class of anti-inflammatory drugs may be used to treat inflammatory bowel disease (IBD).
IBD describes a group of commonly occurring and severe diseases including Crohn's disease and ulcerative colitis. Treatment options for the hallmark symptom of chronically inflamed intestinal tissues are limited, often ultimately requiring surgical removal of inflamed tissue.
A research team led by Professor Cormac Taylor, UCD Conway Institute, have previously shown that a class of drugs called hydroxylase inhibitors may provide a new approach to the treatment of IBD. This study now outlines how this occurs at the molecular level.
Hypoxia is a key microenvironmental feature of inflamed tissues that strongly impacts on the inflammatory processes. A family of oxygen-sensing enzymes called HIF-hydroxylases are responsible for controlling the cellular adaptive response to hypoxia.
This new study, led by Prof Cormac Taylor, Dr Eoin Cummins and Dr Carsten Scholz and published in the Proceedings of the National Academy of Sciences, show that hydroxylase inhibitors work by blocking a pro-inflammatory pathway termed the IL-1 pathway; a key driver of inflammation.
These results give significant new information as to a new level of crosstalk between hypoxia and inflammation and provide a mechanism to explain how this new approach to the control of inflammation may work.
Outlining the results, Dr Eoin Cummins said, "We demonstrate that pharmacologic hydroxylase inhibition down-regulates IL-1b-induced pro-inflammatory NF-kB activity both in vitro and in vivo. Two distinct hydroxylase isoforms, PHD1 and FIH, are acting together to achieve this inhibitory effect, which occurs downstream of TRAF6 activation.
A number of key proteins in the proximal IL-1b signalling pathway were found to interact with PHD1 and FIH and/or be subject to hydroxylation. Based on this data, we hypothesise a key role for hydroxylation as a new post-transcriptional modification in the IL-1b pathway."
"This research stems from studies in our laboratory over the last decade into how cells respond to decreased oxygen levels. We found that cells can adapt to low oxygen levels much like mountain climbers adapt to low oxygen levels at altitude. If we use drugs to mimic this adaptive response in inflammation, it suppresses the inflammatory response" says Professor Taylor.
More information: Regulation of IL-1β–induced NF-κB by hydroxylases links key hypoxic and inflammatory signaling pathways. Carsten C. Scholz, Miguel A. S. Cavadas, Murtaza M. Tambuwala, Emily Hams, Javier Rodríguez, Alex von Kriegsheim, Philip Cotter, Ulrike Bruning, Padraic G. Fallon, Alex Cheong, Eoin P. Cummins, and Cormac T. Taylor. PNAS 2013 ; published ahead of print October 21, 2013, DOI: 10.1073/pnas.1309718110















