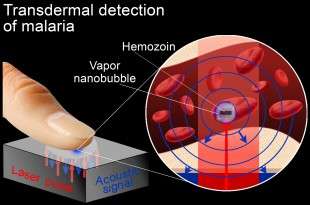
Vapor nanobubbles rapidly detect malaria through the skin
(Medical Xpress)—Rice University researchers have developed a noninvasive technology that accurately detects low levels of malaria infection through the skin in seconds with a laser scanner. The "vapor nanobubble" technology requires no dyes or diagnostic chemicals, and there is no need to draw blood.
A preclinical study published this week in the Proceedings of the National Academy of Sciences shows that Rice's technology detected even a single malaria-infected cell among a million normal cells with zero false-positive readings.
The new diagnostic technology uses a low-powered laser that creates tiny vapor "nanobubbles" inside malaria-infected cells. The bursting bubbles have a unique acoustic signature that allows for an extremely sensitive diagnosis.
"Ours is the first through-the-skin method that's been shown to rapidly and accurately detect malaria in seconds without the use of blood sampling or reagents," said lead investigator Dmitri Lapotko, a Rice scientist who invented the vapor nanobubble technology. The diagnosis and screening will be supported by a low-cost, battery-powered portable device that can be operated by nonmedical personnel. One device should be able to screen up to 200,000 people per year, with the cost of diagnosis estimated to be below 50 cents, he said.
Malaria, one of the world's deadliest diseases, sickens more than 300 million people and kills more than 600,000 each year, most of them young children. Despite widespread global efforts, malaria parasites have become more resistant to drugs, and efficient epidemiological screening and early diagnosis are largely unavailable in the countries most affected by the disease.
Inexpensive rapid diagnostic tests exist, but they lack sensitivity and reliability. The gold standard for diagnosing malaria is a "blood smear" test, which requires a sample of the patient's blood, a trained laboratory technician, chemical reagents and high-quality microscope. These are often unavailable in low-resource hospitals and clinics in the developing world.
"The vapor nanobubble technology for malaria detection is distinct from all previous diagnostic approaches," said study co-author Dr. David Sullivan, a malaria clinician and researcher at Malaria Research Institute at Johns Hopkins University. "The vapor nanobubble transdermal detection method adds a new dimension to malaria diagnostics, and it has the potential to support rapid, high-throughput and highly sensitive diagnosis and screening by nonmedical personnel under field conditions."
The transdermal diagnostic method takes advantage of the optical properties and nanosize of hemozoin, a nanoparticle produced by a malaria parasite inside red blood cell. Hemozoin crystals are not found in normal red blood cells.
Lapotko, a faculty fellow in biochemistry and cell biology and in physics and astronomy at Rice, and lead co-author Ekaterina Lukianova-Hleb found that hemozoin absorbs the energy from a short laser pulse and creates a transient vapor nanobubble. This short-lived vapor nanobubble emerges around the hemozoin nanoparticle and is detected both acoustically and optically. In the study, the researchers found that acoustic detection of nanobubbles made it possible to detect malaria with extraordinary sensitivity.
"The nanobubbles are generated on demand and only by hemozoin," said Lukianova-Hleb, a research scientist in biochemistry and cell biology at Rice. "For this reason, we found that our tests never returned a false-positive result, one in which malaria was mistakenly detected in a normal uninfected cell."
More information: "Hemozoin-generated vapor nanobubbles for transdermal reagent- and needle-free detection of malaria," by Ekaterina Y. Lukianova-Hleb et al,.www.pnas.org/cgi/doi/10.1073/pnas.1316253111


















