Researchers test treatment that can halt acute myeloid leukemia
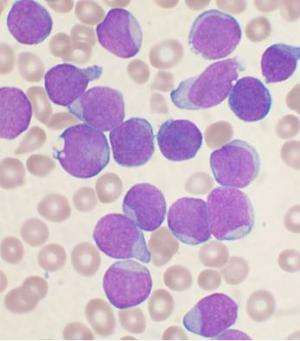
Acute myeloid leukemia is a conundrum among cancers. Immature cells swamp the bone marrow, crowd out healthy cells, and all too often can have devastating consequences.
But a medical investigator at Cold Spring Harbor Laboratory in New York working with a team of researchers has zeroed in on what he calls the malignancy's Achilles' heel - a vulnerable "on" switch driving the cancer. And through sheer happenstance, Dr. Christopher Vakoc, the physician-scientist leading the research, identified a potential therapy that flips the switch off. It's still far too early to say whether the approach works.
This tough-to-treat cancer, like other recalcitrant malignancies, is under study on the 120-acre Long Island campus where scientists are unmasking aberrant genes and exposing previously unsuspected protein pathways linked to cancer. Vakoc has found other "small molecules" associated with the leukemia and is on the hunt for others.
Early clinical trials of therapeutics that turn off the molecular "on" switch of the cancer - widely known as AML - are underway.
The Leukemia and Lymphoma Society of America, the nation's leading advocacy organization for patients, applauds Vakoc and his nationwide team of collaborators. The society says there hasn't been a new therapeutic approach to the disease in more than three decades.
On Tuesday, Vakoc will be recognized by the American Association for Cancer Research during its annual meeting in Philadelphia. He will receive the Outstanding Achievement in Cancer Research Award, an honor won by other researchers who have gone on to win the Nobel Prize.
"What makes AML unique" among leukemias, Vakoc said, "is its acute property. Someone can go from being totally healthy and active to having their bone marrow overcome by leukemic cells.
"There are other leukemias that are chronic and smoldering, but the hallmark of this disease is the acute aspect of it," Vakoc said.
Acute myeloid leukemia chokes off the ability to generate a healthy blood supply. It is defiantly incurable in about 70 percent of patients, and more than 10,000 people die of AML annually nationwide.
Vakoc exposed the infinitesimal protein - BRD4 - at the heart of AML in 2010. With BRD4 in hand, Vakoc had found what he calls "a druggable target."
"Using DNA-based techniques, we could show that BRD4 was an awesome target, representing an Achilles' heel in AML," Vakoc said.
"However, in the early days of these efforts, we didn't know if a drug would be available that actually targets and exploits the BRD4 vulnerability.
"Serendipitously, a paper was published while we were studying BRD4 that described the first drugs that interfere with it, developed by a chemist at Harvard. We immediately got in touch with him and discovered, quite to our amazement, that his drugs had robust effects in treating leukemia in mice."
For decades, cancers of all kinds have been cured in mice, but when scientists scaled up the evolutionary tree to humans, their once-wondrous medications failed to effectively quell the disease. There is a hint of good news, however, in the human clinical research.
Phase I clinical trials are being overseen by four pharmaceutical companies: Oncoethix, Constellation, Tensha Therapeutics and GlaxoSmithKline. Trials began in 2013 and 2014, Vakoc said.
"These are first-in-human dose-escalation trials to evaluate safety of these compounds," he said. He estimates about 100 people with AML have received the experimental medications to date.
Oncoethix has already reported its Phase I data and shown the approach to be safe. Study participants, Vakoc said, found their leukemic cells "were eliminated and normal blood production resumed."
"These are promising initial findings, but are in no way conclusive," he said. "In the coming years, we will see these drugs rigorously evaluated in Phase II, and hopefully, Phase III clinical studies, perhaps in combination with other drugs."
The research is being closely watched by the Leukemia and Lymphoma Society.
"There have been almost no advances in the standard of therapy for patients with AML in more than 30 years," Andrea Greif, society spokeswoman, said. "So any new finding that brings us closer to understanding the underpinnings of the causes of AML and developing new therapies to target molecular aberrations in AML is certainly encouraging news for the patients we serve," Greif said.
Vakoc's advances against the aggressive cancer are proceeding as Cold Spring Harbor Laboratory has committed to a historic agreement that will bring its groundbreaking research to the bedsides of patients in the North Shore-Long Island Jewish Health System.
The pact is a $120 million collaboration involving the development of clinical trials and treatment strategies for a variety of cancers based on the laboratory's most promising investigations.
Neither institution has yet announced which trials will be among the first offered to North Shore-LIJ patients. A clinical study of an aggressive form of breast cancer was underway before the collaborative agreement was announced.
Cancer experts at both institutions are riveted on the development of targeted therapies. These medications home in on specific molecular mechanisms - weak spots - in cancer cells, like the molecule dubbed BRD4, identified by Vakoc as a bull's-eye to target in AML.
"Traditionally, we have treated cancer by interfering with the mechanism of cell division," said Dr. George Raptis, vice president of North Shore's Cancer Institute in Lake Success, referring to chemotherapy. He describes chemo as indiscriminate - killing cancer cells but often scathing healthy ones in the process.
"Cancer cells divide quickly and are more amenable to being destroyed by these drugs," he said of chemo. "But with an increasing understanding of cancer on a molecular and genetic level, we are now able to find not one but numerous Achilles' heels."
The hope, Raptis said, is to gain more precision treating cancers of all kinds through translational medicine - bringing what is learned in the lab directly to patients.
Raptis describes researchers at Cold Spring Harbor Laboratory on parallel missions - searching for specific vulnerabilities in cancer cells while simultaneously hunting for medications to assault those sites.
Vakoc's investigations are among numerous cancer studies underway at the laboratory, situated on a hilly and deeply arbored campus overlooking the harbor. The lab is celebrating its 125th anniversary this year.
Dr. David Tuveson is studying cancer of the pancreas and working on a possible diagnostic for the disease. Dr. Raffaella Sordella is delving into the causes of drug-resistant lung cancer.
Last year, Dr. Mikala Egeblad won a highly coveted $2.5 million breast cancer research award from the Department of Defense. Another breast cancer researcher, Dr. Nicholas Tonks, is exploring drug resistance in an aggressive form of the disease.
"What we're doing is working on alternative strategies, some of the things that industry is not doing," Tonks said.
©2015 Newsday
Distributed by Tribune Content Agency, LLC
















