Discovery of a new drug target could lead to novel treatment for severe autism
Penn State University scientists have discovered a novel drug target and have rescued functional deficits in human nerve cells derived from patients with Rett Syndrome, a severe form of autism-spectrum disorder. The research, led by Gong Chen, professor of biology and the Verne M. Willaman Chair in Life Sciences at Penn State, could lead to a new treatment for Rett Syndrome and other forms of autism-spectrum disorders. A paper describing the research will be published on January 4, 2016 in the online Early Edition of the journal Proceedings of the National Academy of Sciences.
"The most exciting part of this research is that it directly uses human neurons that originated from Rett Syndrome patients as a clinically-relevant disease model to investigate the underlying mechanism," said Dr. Chen. "Therefore, the new drug target discovered in this study might have direct clinical implication in the treatment of Rett Syndrome and potentially for other autism-spectrum disorders as well."
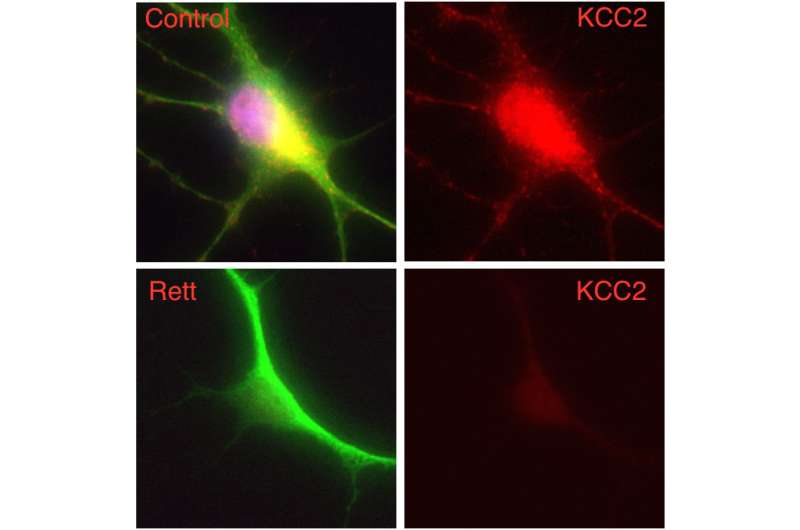
The researchers differentiated stem cells derived from the skin cells of patients with Rett Syndrome into nerve cells that could be studied in the laboratory. These nerve cells carry a mutation in the gene MECP2, and such gene mutations are believed to be the cause of most cases of Rett Syndrome. The researchers discovered that these nerve cells lacked an important molecule, KCC2, that is critical to normal nerve cell function and brain development.
"KCC2 controls the function of the neurotransmitter GABA at a critical time during early brain development," Chen said. "Interestingly, when we put KCC2 back into Rett neurons, the GABA function returns to normal. We therefore think that increasing KCC2 function in individuals with Rett Syndrome may lead to a potential new treatment."
The researchers also showed that treating diseased nerve cells with insulin-like growth factor 1 (IGF1) elevated the level of KCC2 and corrected the function of the GABA neurotransmitter. IGF1 is a molecule that has been shown to alleviate symptoms in a mouse model of Rett Syndrome and is the subject of an ongoing phase-2 clinical trial for the treatment of the disease in humans.
"The finding that IGF1 can rescue the impaired KCC2 level in Rett neurons is important not only because it provides an explanation for the action of IGF1," said Xin Tang, a graduate student in Chen's Lab and the first-listed author of the paper, "but also because it opens the possibility of finding more small molecules that can act on KCC2 to treat Rett syndrome and other autism spectrum disorders."
More information: KCC2 rescues functional deficits in human neurons derived from patients with Rett syndrome, Proceedings of the National Academy of Sciences, www.pnas.org/cgi/doi/10.1073/pnas.1524013113
















