New HPV vaccine could curb cervical cancers and health costs if adopted widely
A Yale-led study finds that a new vaccine for human papillomavirus (HPV) would significantly reduce both cervical cancer incidence and healthcare costs if states coordinated policies to improve coverage.
The study was published April 18 by Proceedings of the National Academy of Sciences.
HPV, the most common sexually transmitted infection in the United States, is the primary cause of cervical cancer. A new vaccine available since 2015, Gardasil 9, provides protection against nine different HPV types, including five cancer-causing types that were not included in older vaccines. A team of researchers at Yale School of Public Health and the University of Waterloo developed a transmission model to determine the potential impact of the vaccine on cervical cancer incidence and healthcare costs.
The novel model took into account several factors affecting HPV transmission and cervical cancer progression. It incorporated 10 HPV types, demographics, age, sexual behavior, as well as state-specific vaccine policy and migration patterns.
The researchers found that switching to Gardasil 9 would result in greater health benefits at the same or lower cost. Specifically, the new vaccine would decrease cervical cancer incidence by 73%, compared to 63% with the older vaccines, and reduce mortality by 49% versus 43%.
The study also determined that these improvements could be realized at the same or lower cost despite the higher per-dose cost of Gardasil 9. Notably, their finding of increased cost-effectiveness holds whether vaccination rates increase or stay the same, said first author David Durham, associate research scientist at the Center for Infectious Disease Modeling and Analysis (CIDMA) at Yale School of Public Health. "Adopting the new vaccine is always cost-effective relative to the old vaccines," he noted.
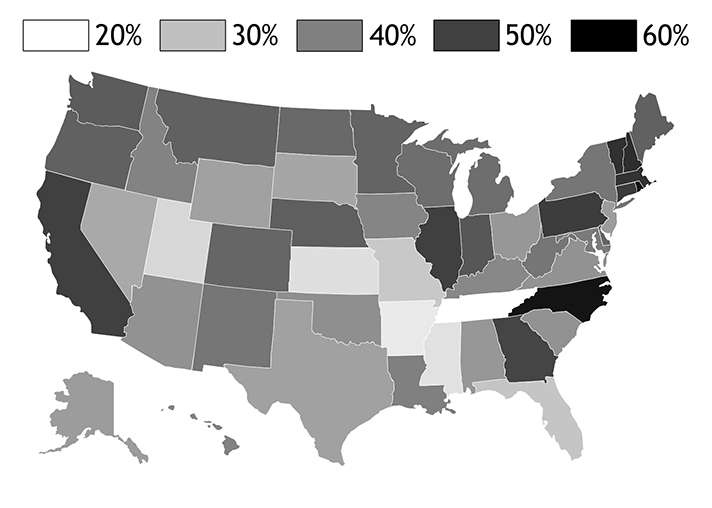
In addition, efforts to expand HPV vaccination, particularly in states with low coverage, could prevent even more cancers and deaths, said the researchers, adding that due to interstate migration, all states would benefit if they aligned vaccination policy. "The greatest benefits of HPV vaccination both in terms of cancer reduction and health care costs are realized when policy promoting vaccination is coordinated across states," said Alison Galvani, the Burnett and Stender Families Professor of Epidemiology and director of CIDMA.
Furthermore, increased funding to states could improve vaccine coverage and public health, the researchers noted. Durham pointed to funds provided by states and the Centers for Disease Control and Prevention's (CDC) Prevention and Public Health Fund. More resources "do lead to improvements in coverage," he said. "In terms of number of cancers averted per vaccine, there are decreasing marginal returns in states that already have high coverage. You get more bang for your buck by focusing first on states with lower coverage."
The CDC currently recommends vaccination for females aged 11-26 and males aged 11-21. Three doses are recommended for lasting protection against cervical cancer, the researchers said. HPV is common in both males and females, and can cause cancers of the anus, mouth/throat and penis in males.
More information:
National- and state-level impact and cost-effectiveness of nonavalent HPV vaccination in the United States, Proceedings of the National Academy of Sciences,
www.pnas.org/cgi/doi/10.1073/pnas.1515528113


















