A gene that fights cancer, but causes it too
An international team of researchers, led by scientists at the University of California, San Diego School of Medicine, and the Eastern Hepatobiliary Surgery Hospital in China, say a human gene implicated in the development of leukemia also acts to prevent cancer of the liver.
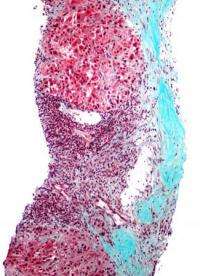
Writing in the May 17 issue of the journal Cancer Cell, Gen-Sheng Feng, PhD, UCSD professor of pathology, and colleagues in San Diego, Shanghai and Turin report that an enzyme produced by the human gene PTPN11 appears to help protect hepatocytes (liver cells) from toxic damage and death. Conversely, the same enzyme, called Shp2, is a known factor in the development of several types of leukemia.
"The new function for PTPN11/Shp2 as a tumor suppressor in hepatocellular carcinoma (HCC) stands in contrast to its known oncogenic effect in leukemogenesis," said Feng. "It's a surprising finding, but one that we think provides a fresh view of oncogenesis. The same gene can have oncogenic or anti-oncogenic effects, depending upon cellular context."
Previous studies had determined that PTPN11 was a proto-oncogene. That is, dominant active mutations in the gene had been identified in several types of leukemia patients, as was an over-expression of the gene product Shp2. Feng and colleagues looked to see what happened when Shp2 was knocked out specifically in hepatocytes in a mouse model.
The result wasn't good: The mice got liver cancer.
Strikingly, deficient or low expression of PTPN11 was detected in a sub-fraction of human HCC patient samples by researchers at the Eastern Hepatobiliary Surgery Hospital in Shanghai, China. That work was led by Hongyang Wang, MD, PhD and a professor of molecular biology.
"The liver is a most critical metabolic organ in mammals, including humans," said Feng. "It has a unique regenerative capacity that allows it to resist damage by food toxins, viruses and alcohol. Shp2 normally acts to protect hepatocytes. Removing Shp2 from these liver cells leads to their death, which in turn triggers compensatory regeneration and inflammatory responses. That results in enhanced development of HCC induced by a chemical carcinogen."
Feng said the findings highlight the unique mechanism underlying HCC, but more broadly, they reveal new complexities in how different types of cancer begin. Indeed, the researchers say their work also uncovered pro- and anti-oncogenic activities in a gene transcription factor called Stat3.
"Our results indicate a requirement for Stat3 in promoting HCC development, which is consistent with the literature saying Stat3 is pro-oncogenic. But we also found that deletion of Stat3 in hepatocytes resulted in a modest, but significant, increase in HCC."
Feng said the findings underscore the need for caution in designing therapeutic strategies for treating HCCs and other types of cancers because the answer might also be the problem.














