Uncovering a key player in metastasis
About 90 percent of cancer deaths are caused by secondary tumors, known as metastases, which spread from the original tumor site.
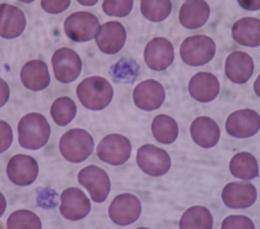
To become mobile and break free from the original tumor, cancer cells need help from other cells in their environment. Many cells have been implicated in this process, including immune system cells and cells that form connective tissue. Another collaborator in metastasis is platelets, the blood cells whose normal function is to promote blood clotting.
The exact role played by platelets has been unclear, but a new paper from Richard Hynes, the Daniel K. Ludwig Professor for Cancer Research, and colleagues shows that platelets give off chemical signals that induce tumor cells to become more invasive and plant themselves in new locations. The findings, published Nov. 14 in Cancer Cell, may help researchers develop drugs that could prevent cancers from spreading, if they are diagnosed before metastasis occurs.
For many years, cancer biologists believed that platelets helped to promote metastasis by helping the cells to form big clumps, allowing them to get stuck in new locations more easily. However, some suspected they might have a more active role, because they contain many growth factors and cytokines, many of which can stimulate cancerous growth.
Before cancer cells can metastasize, they typically undergo a shift known as the epithelial-mesenchymal transition (EMT). During this shift, cells lose their ability to adhere to each other and begin to migrate away from their original locations.
Myriam Labelle, a postdoc in Hynes’ lab and lead author of the Cancer Cell paper, found that cancer cells would undergo this transition if grown in contact with platelets in a lab dish. She then analyzed which genes were being turned on in the metastatic cells and found that genes activated by transforming growth factor beta (TGF-beta, or TGF-b) were very active. TGF-beta was already known to promote EMT. Labelle then went on to show that depletion of TGF-beta from platelets in vivo blocked metastasis.
“This work shows that platelets are not just a shield for circulating cancer cells, but also a traveling kit of pro-invasive stimuli,” says Joan Massagué, chair of the cancer biology and genetics program at the Sloan-Kettering Institute, who was not part of this study. “For nearly three decades platelets have been known to be the richest source of TGF-b in the body, yet it is only now that someone realized what an important role platelets play as a TGF-b source in tumor dissemination.”
A complex interaction
In further experiments, Labelle found that the cancer cells would not become metastatic if exposed only to TGF-beta, suggesting that they need an additional signal from the platelets.
Platelets release many chemicals other than TGF-beta — they are “little bags of stickiness and growth factors,” designed to promote wound healing, says Hynes, who is a member of the David H. Koch Institute for Integrative Cancer Research at MIT. However, none of those chemicals on its own was enough to promote metastasis. Labelle found that direct physical contact between platelets and tumor cells was necessary for the cells to become metastatic.
Specifically, when platelets come into contact with tumor cells, they somehow activate the NF-kappa-b pathway, which is involved in regulating the immune response to infection. Both of the signals, NF-kappa-b activation and TGF-beta, are necessary for the switch to occur.
While tumor cells receive the initial stimulus to become mobile while still in their original location, Hynes and Labelle suspect that the additional boost they get from platelets once they enter the bloodstream makes it easier for the cells to penetrate the walls of blood vessels into a new tumor site.
White blood cells are also suspected in promoting metastasis, and Labelle is now doing experiments to figure out what their role may be, and how they may work together with platelets. She is also examining how platelets activate the NF-kappa-b pathway in tumor cells.
Better understanding of the signals that tumor cells need to metastasize may help researchers develop drugs that can prevent such metastases from developing. “It’s important to understand exactly what platelets are doing, and eventually this could be an opportunity for drugs that would treat metastasis,” Labelle says.
Such an approach would be useful for stopping primary tumors or metastases from spreading, but would likely not have much effect on secondary tumors that had already formed.
This story is republished courtesy of MIT News (web.mit.edu/newsoffice/), a popular site that covers news about MIT research, innovation and teaching.














