Inner weapons against allergies: Gut bacteria control allergic diseases
When poet Walt Whitman wrote that we "contain multitudes," he was speaking metaphorically, but he was correct in the literal sense. Every human being carries over 100 trillion individual bacterial cells within the intestine -- ten times more cells than comprise the body itself.
Now, David Artis, PhD, associate professor of Microbiology, along with postdoctoral fellow David Hill, PhD, from the Perelman School of Medicine at the University of Pennsylvania, and collaborators from The Children's Hospital of Philadelphia and institutions in Japan and Germany, have found that these commensal bacteria might play an important role in influencing and controlling allergic inflammation. The commensal relationship that develops between humans and internal bacteria is one in which both humans and bacteria derive benefits.
The study -- appearing this week in Nature Medicine -- suggests that therapeutic targeting of immune cell responses to resident gut bacteria may be beneficial in treating allergic diseases.
The researchers build on previous work demonstrating that selective manipulation of the commensal bacterial population could affect the immune system. "Studies in human patients suggest that changes in commensal populations or exposure to broad spectrum antibiotics can predispose patients to the development of systemic allergic diseases," Hill explains. "In addition, previous studies in animal models have shown that commensal bacteria can influence local immune cells in the intestine. However, the cellular and molecular mechanisms by which commensal bacteria influence the host immune system, in particular the branches of the host immune system that regulate allergic inflammation, are not well understood."
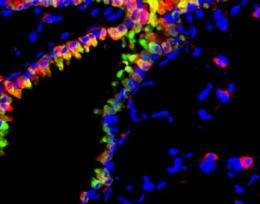
Artis and his colleagues focused on the role of basophils, a type of white blood cell, in causing allergic inflammation, and the relationship between basophil responses and allergic disease.
The investigators administered broad-spectrum oral antibiotics to deplete certain types of bacteria in mice and to subsequently examine the affects on levels of circulating basophils in the blood. Using an animal-based model of allergic inflammation in the lung that shares characteristics with asthma in humans, they found that antibiotic treatment resulted in significantly elevated basophil responses and a marked increase in the amount of basophil-mediated allergic airway inflammation. Elevated serum levels of IgE, an important mediator in allergic disease, were also observed.
After the antibiotic-treated mice were exposed to house dust mite allergen (HDM), a human allergen and a model of allergic airway disease in mice, they showed higher basophil responses in the blood and lymph nodes as well as a heightened allergic response with increased inflammation in the lungs.
Germ-free mice, which are reared in a sterile environment and thus lack all live commensal bacteria, also showed similar responses to those observed in antibiotic-treated mice when exposed to HDM. This finding indicates that commensal bacteria-derived signals are responsible for maintaining normal basophil numbers in the steady-state.
Artis and his colleagues also found that serum concentrations of IgE and circulating basophil numbers were limited by B cell-intrinsic expression of myeloid differentiation factor 88 (MyD88), a protein known to play a role in the recognition of bacteria-derived factors. Signals derived from the commensal bacteria were found to act via IgE to control the number of circulating basophils by limiting the proliferation of basophil precursor cells in the bone marrow.
All of these findings indicate important new processes by which resident commensal bacterial populations influence and control basophil responses and thus influence the response to allergens in our environment.
"The identification of a mechanistic connection between commensal bacteria, basophils, and allergic disease illuminates several new avenues that could be targeted by future therapeutics to block or inhibit the development of allergic disease," Artis notes. Further study and identification of these commensal pathways could also have implications for other chronic diseases related to immune system functioning.
Artis and his colleagues hope to further understand this intricate interplay between the immune system and commensal bacteria. "It may be beneficial to identify the specific commensals and commensal-derived signals that regulate circulating basophil populations as this could lead to the development of new probiotic or other commensal-derived therapies," he says. The work makes clear that the bacterial multitudes within our bodies may have a function and a value never before appreciated.















