Cancer data in the 'cloud' could lead to more effective treatment
Storing music and photos on distant computers via "cloud" technology is nothing new. But Johns Hopkins researchers are now using this tactic to collect detailed information from thousands of cancer cell samples. The goal is to help doctors make better predictions about how a patient's illness will progress and what type of treatment will be most effective.
The project, supported by a new $3.75 million National Cancer Institute grant, was launched because researchers now realize that cancer cells affecting the same type of tissue can behave differently in different patients. Prostate cancers may grow rapidly in one patient, but expand at a glacial pace in another. A drug that kills a tumor in one patient may be useless or even harmful in the next patient.
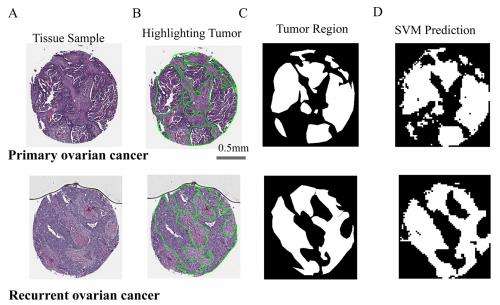
To help doctors prepare a more personalized medical prognosis and treatment plan, Johns Hopkins has assembled experts in cancer and engineering, led by Denis Wirtz , associate director of the university's Institute for NanoBioTechnology. The team has begun characterizing and storing cancer data collected through a process called high-throughput cell phenotyping.
"We use scanning microscopy to take pictures of the size and shape of cancer cells," said Wirtz, who also directs the Johns Hopkins Physical Sciences-Oncology Center. "We also extract information about what is happening inside the cells and at the genetic level. We make notes of the age and gender of the patient and any treatment received. Looked at as a whole, this information can help us identify a 'signature' for a certain type of cancer.
That gives us a better idea of how it spreads and how it responds to certain drugs." He added, "The long-range goal is to make this data available through the Internet to physicians who are diagnosing and treating cancer patients around the world."
Wirtz , a professor of chemical and biomolecular engineering in the university's Whiting School of Engineering, has been working with School of Medicine researchers Ralph Hruban and Anirban Maitra to begin the database with material from the files of thousands of cancer patients who have been evaluated and treated at Johns Hopkins. The patients' personal information has been deleted, but the remaining medical case data allows the researchers to trace the course of the disease from initial testing through treatment and outcome.
"This technology may provide a way to centralize specimen data, images and analysis in a way that hasn't been done before," said Maitra, a professor of pathology and oncology, "and we'll be using the information now to find better ways to treat disease."
The Johns Hopkins team will soon collect similar data from other major U.S. cancer research centers that are also supported by the National Institutes of Health. The initial focus will be pancreatic cancer, which is particularly aggressive and lethal.
"We may be able to correlate DNA changes that occur in individual pancreatic cancer cells with the appearance of these cells at the cellular level," said Hruban, a professor of pathology and oncology and director of the Sol Goldman Pancreatic Cancer Research Center. "The potential for this approach to provide insight into the fundamental biology of pancreatic cancer is significant, as are the potential clinical applications in predicting a patient's prognosis and in guiding therapy."
Other types of the disease, including breast and prostate cancer, will be addressed in the near future. Early data is being stored on computers at the Los Alamos National Laboratory under an arrangement funded by the NIH.
According to Wirtz, the details recorded in the online database will differ from those produced in traditional biopsy evaluations. Typically, information about a patient's disease is obtained by averaging the results from trillions of cells that have been blended together.
With the new scanning system, however, the Johns Hopkins researchers will obtain views of individual cells retrieved from individual patients, even from different parts of the same organ.
This ability to examine single cells is important, Wirtz said, because scientists have discovered that even cells that possess the identical genetic makeup can vary in other small ways that affect the behavior of cancer. For example, these tiny variations in genetically identical cells can cause some to be vulnerable to a particular cancer drug.
"We've come to realize that it is the heterogeneity—the diversity of cells that have different characteristics—that is important in evaluating a cancer case," Wirtz said. "In the end, what matters is the cell properties. That's what we measure."
Researchers will begin their studies on clinical samples collected at Johns Hopkins to determine how well the technology works and validate it's potential before it can be used to aid clinical decision-making.
The software and hardware used in the high-throughput cell phenotyping process is protected by patents obtained through the Johns Hopkins Technology Transfer office. The $3.75 million National Cancer Institute grant (CA174388) will be disbursed to the Johns Hopkins Institute for NanoBioTechnology over a five-year period. The funds were allocated through the National Institutes of Health's Common Fund Single Cell Analysis Program.














