Blocking molecular pathway reverses pulmonary hypertension in rats
Pulmonary hypertension, a deadly form of high blood pressure that develops in the lungs, may be caused by an inflammation-producing molecular pathway that damages the inner lining of blood vessels, according to a new study by researchers at the Stanford University School of Medicine.
The results, which will be published Aug. 28 in Science Translational Medicine, suggest that using medications to block this pathway could lead to the first-known cure for the disease, apart from lung transplantation. The new research could also lead to a better understanding of other diseases involving inflammation of blood vessels, such as coronary artery disease, said Mark Nicolls, MD, senior author of the study and division chief of pulmonary and critical care medicine at Stanford, as well as a staff physician at the Veterans Affairs Palo Alto Health Care System.
"We believe that targeting inflammation is an exciting approach to augment current treatments for pulmonary hypertension because it may reverse the underlying cause of the disease," said Nicolls, who is also director of the Lung Immunology Program and an associate professor of medicine. "We believe this is going to be an approach that helps a large number of patients."
The lead author of the study is Wen Tian, PhD, a research associate in Nicolls' lab.
Pulmonary hypertension, while rare, usually strikes young and middle-aged women, leaving them short of breath and often unable to complete simple daily tasks. The condition can be fatal. The risk is higher for people with certain autoimmune diseases (such as scleroderma or lupus), HIV, congenital heart disease or liver disease. The risk also is higher for those who have used street drugs, such as amphetamines or cocaine, or the diet drug fenphen.
About 100,000 people in the United States and Europe have been diagnosed with pulmonary hypertension, but many others are believed to go undiagnosed because the main symptom, shortness of breath, is nonspecific. Until the 1990s, there were no treatments except lung transplantation, which has varying degrees of success.
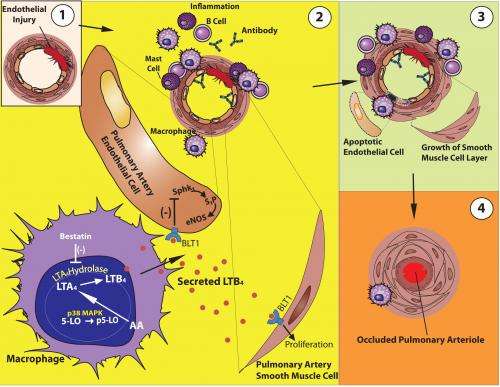
What is known about the disease is that the narrowing of blood vessels in the lungs is caused by a mysterious proliferation of the smooth muscle cells that ring those vessels. As the vessel walls thicken, they become increasingly occluded, choking off blood flow.
Blood vessels are elastic tubes that have an outer layer of smooth muscle and an inner layer of endothelial cells. The current treatment for patients with pulmonary hypertension is vasodilators, drugs that cause smooth muscle cells to relax, permitting more blood to flow through the diseased vessels. These drugs help to extend survival and relieve some symptoms, but they don't provide a cure.
"Current approved therapies for pulmonary hypertension have focused on dilating blood vessels without special attention being paid to the inflammation that is frequently seen around blood vessels," Nicolls said. "We were interested in finding out how inflammation contributes to the disease."
In laboratory experiments, researchers removed inflammation-producing cells called macrophages from the lung tissue of rats dying of pulmonary hypertension and put the cells in cultures with healthy rat endothelial cells.
"We were shocked to find that half of the endothelial cells were dead within 24 hours," Nicolls said. "That totally surprised us."
In subsequent lab experiments, researchers found that if they blocked the molecular pathway triggered by the macrophages, the endothelial cells didn't die. Researchers conducted similar experiments in human tissue taken from the diseased lungs of patients. The results were similar. "The same pathways were at play in the human lungs," Nicolls said.
In experiments in live rats with induced pulmonary hypertension, the disease was reversed when researchers blocked the inflammation-producing pathway.
"It was dramatic," Nicolls said. "We could start the drug as late as three weeks when animals were breathing hard and walking slowly, and the disease reversed."
More information: "Blocking Macrophage Leukotriene B4 Prevents Endothelial Injury and Reverses Pulmonary Hypertension," by W. Tian et al. Science Translational Medicine, 2013.
















