November 26, 2013 report
Viral replication may not be primary cause of HIV-1 persistence in patients receiving cART
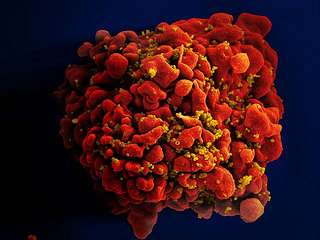
(Medical Xpress)—A team of researchers with members from Europe and the U.S. has found that viral replication may not be the main reason that the HIV virus is able to persist in the cells of infected patients for many years. In their paper published in Proceedings of the National Academy of Sciences, the researchers outline a study they conducted with volunteer HIV infected patients and the results they found that indicated there is likely another cause for the long term persistence of HIV in human patients.
Over the years since the HIV virus made itself known in the form of AIDS, medical researchers have made dramatic gains in treating the disease. No longer is a positive test a death sentence. This has been made possible by the development of a cocktail of drugs known collectively as combinational antiretroviral therapy (cART). While it doesn't wipe the virus from the body, it does chase it into hiding. What has confounded researchers is the mechanism by which the virus hides in the body—quite often for several years, before suddenly one day revealing itself in the form of an outbreak. As part of this new effort, the research team believes they have taken a step forward in understanding how the HIV virus hides, and then, what causes it to become active again.
In the study, eight HIV positive patients who had been receiving cART for at least 12 years, volunteered to assist in the research effort. Each gave blood samples which were analyzed in a new way. In so doing the researchers found that each of the patients had a pool of infected CD4 cells—they are responsible for alerting T-cells when a foreign body is detected. The HIV virus had inserted its DNA into such cells in just such a way as to allow it to remain hidden in the body for long periods of time. It was only when some other foreign element entered the system that the CD4 cells were engaged. That in turn set off the HIV virus cells.
This, the researchers suggest, explains why a patient can go for years without any noticeable signs of HIV, then one day suddenly have a blow up. It's because some other virus or bacteria has made its way into the body causing the immune system to go on the attack. When it did so, it unwitting unleashed the HIV virus cells as well.
The researcher's findings suggest that the HIV virus doesn't need to replicate to remain active in the body for long periods of time as has been suspected.
More information: The HIV-1 reservoir in eight patients on long-term suppressive antiretroviral therapy is stable with few genetic changes over time, Published online before print November 25, 2013, DOI: 10.1073/pnas.1308313110
Abstract
The source and dynamics of persistent HIV-1 during long-term combinational antiretroviral therapy (cART) are critical to understanding the barriers to curing HIV-1 infection. To address this issue, we isolated and genetically characterized HIV-1 DNA from naïve and memory T cells from peripheral blood and gut-associated lymphoid tissue (GALT) from eight patients after 4–12 y of suppressive cART. Our detailed analysis of these eight patients indicates that persistent HIV-1 in peripheral blood and GALT is found primarily in memory CD4+ T cells [CD45RO+/CD27(+/−)]. The HIV-1 infection frequency of CD4+ T cells from peripheral blood and GALT was higher in patients who initiated treatment during chronic compared with acute/early infection, indicating that early initiation of therapy results in lower HIV-1 reservoir size in blood and gut. Phylogenetic analysis revealed an HIV-1 genetic change between RNA sequences isolated before initiation of cART and intracellular HIV-1 sequences from the T-cell subsets after 4–12 y of suppressive cART in four of the eight patients. However, evolutionary rate analyses estimated no greater than three nucleotide substitutions per gene region analyzed during all of the 4–12 y of suppressive therapy. We also identified a clearly replication-incompetent viral sequence in multiple memory T cells in one patient, strongly supporting asynchronous cell replication of a cell containing integrated HIV-1 DNA as the source. This study indicates that persistence of a remarkably stable population of infected memory cells will be the primary barrier to a cure, and, with little evidence of viral replication, this population could be maintained by homeostatic cell proliferation or other processes.
© 2013 Medical Xpress
















