Sleep-deprived mice show connections among lack of shut-eye, diabetes, age
Sleep, or the lack of it, seems to affect just about every aspect of human physiology. Yet, the molecular pathways through which sleep deprivation wreaks its detrimental effects on the body remain poorly understood. Although numerous studies have looked at the consequences of sleep deprivation on the brain, comparatively few have directly tested its effects on peripheral organs.
During sleep deprivation cells upregulate the UPR – the unfolded protein response – a process where misfolded proteins get refolded or degraded.
Five years ago, researchers at the Perelman School of Medicine, University of Pennsylvania, showed that the UPR is an adaptive response to stress induced by sleep deprivation and is impaired in the brains of old mice. Those findings suggested that inadequate sleep in the elderly, who normally experience sleep disturbances, could exacerbate an already-impaired protective response to protein misfolding that happens in aging cells. Protein misfolding and clumping is associated with many diseases such as Alzheimer's and Parkinson's, noted Nirinjini Naidoo, Ph.D., research associate professor in the Division of Sleep Medicine in that study.
Naidoo is also senior author of a follow-up study in Aging Cell this month that shows, for the first time, an effect of sleep deprivation on the UPR in peripheral tissue, in this case, the pancreas. They showed that stress in pancreatic cells due to sleep deprivation may contribute to the loss or dysfunction of these cells important to maintaining proper blood sugar levels, and that these functions may be exacerbated by normal aging.
"The combined effect of aging and sleep deprivation resulted in a loss of control of blood sugar reminiscent of pre-diabetes in mice," says Naidoo. "We hypothesize that older humans might be especially susceptible to the effects of sleep deprivation on the disruption of glucose homeostasis via cell stress."
Working with Penn colleague Joe Baur, Ph.D., assistant professor of Physiology, Naidoo started a collaboration to look at the relationship of sleep deprivation, the UPR, and metabolic response with age. Other researchers had suggested that the death of beta cells associated with type 2 diabetes may be due to stress in a cell compartment called the endoplasmic reticulum (ER). The UPR is one part of the quality control system in the ER, where some proteins are made.
Knowing this, Naidoo and Baur asked if sleep deprivation (SD) causes ER stress in the pancreas, via an increase in protein misfolding, and in turn, how this relates to aging.
The team examined tissues in mice for cellular stress following acute SD, and they also looked for cellular stress in aging mice. Their results show that both age and SD combine to induce cellular stress in the pancreas.
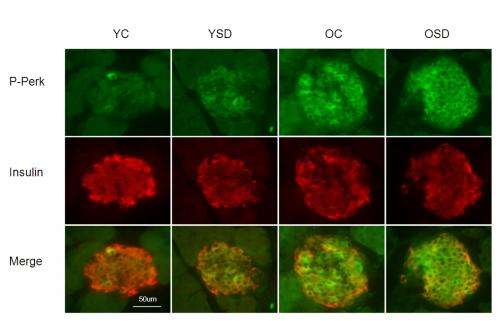
Older mice fared markedly worse when subjected to sleep deprivation. Pancreas tissue from older mice or from young animals subjected to sleep deprivation exhibited signs of protein misfolding, yet both were able to maintain insulin secretion and control blood sugar levels. Pancreas tissue from acutely sleep-deprived aged animals exhibited a marked increase in CHOP, a protein associated with cell death, suggesting a maladaptive response to cellular stress with age that was amplified by sleep deprivation.
Acute sleep deprivation caused increased plasma glucose levels in both young and old animals. However, this change was not overtly related to stress in beta cells, since plasma insulin levels were not lower following acute lack of sleep.
Accordingly, young animals subjected to acute sleep deprivation remained tolerant to a glucose challenge. In a chronic sleep deprivation experiment, young mice were sensitized to insulin and had improved control of their blood sugar, whereas aged animals became hyperglycemic and failed to maintain appropriate plasma insulin concentrations.
While changes in insulin secretion are unlikely to play a major role in the acute effects of SD, cellular stress in pancreatic tissue suggests that chronic SD may contribute to the loss or dysfunction of endocrine cells, and that these effects may be exacerbated by normal aging, say the researchers.
















