A clinical trial to test a new model of an "artificial pancreas" is being pioneered in Spain
The Universitat Politècnica de València, the Instituto de Investigación Sanitaria (INCLIVA) of the Hospital Clínico Universitario de Valencia, the Hospital Clínic de Barcelona and the Polytechnic School of the Universitat de Girona (UdG) have started a clinical trial of healthcare technology being pioneered in Spain, in order to study the efficiency of an artificial pancreas.
The artificial pancreas is a device based on a control mathematical algorithm that calculates the optimal dose of insulin according to the needs of any patient at any time. It consists of providing the insulin pumps used by type 1 diabetes mellitus patients with an additional system (control algorithm) able to indicate the exact quantity of insulin needed by a patient at any time.
The trial is lead by Dr. F. Javier Ampudia-Blasco, from the Endocrinology Department of the Hospital Clínico Universitario (Department Head: Dr. Juan Ascaso), in collaboration with the Dr. Paolo Rossetti, at the Hospital Fransesc de Borja in Gandía and researcher at the INCLIVA. Two engineers are also taking part as the main co-researchers, Jorge Bondia, from the Instituto Universitario de Automática e Informática Industrial of the UPV, and Josep Vehí, from the UdG, as well as Dr. Ignacio Conget, Dr. Marga Giménez and Dr. Carmen Quirós, from the Hospital Clínic de Barcelona.
This trial emerges from a research project that dates back to 2004, when researchers at the Instituto Universitario de Automática e Informática Industrial of the UPV (Jorge Bondia) and at the Institute of Informatics and Applications of the Universitat de Girona (Josep Vehí) decided to search for solutions to one of the biggest problems for diabetes patients: determining the quantity of insulin necessary at any given time.
Currently, according to Jorge Bondia, "the patient undergoes an intensive insulin therapy, either with multiple daily injections or with continuous infusion with insulin pumps. The intensive insulin therapy is very effective, but it causes an increase in hypoglycaemic episodes. Another problem is that very low insulin levels can lead to a diabetic coma." Glycaemia monitoring is a basic element in the treatment and control of diabetic patients.
According to Dr. Ampudia-Blasco, "Type 1 diabetes mellitus is a chronic disease which requires the administration of insulin for life. Today, for those patients who do not achieve an optimum glycaemia control with the administration of multiple insulin injections, the use of insulin pumps or systems of continuous subcutaneous infusion of insulin (ISCI, in Spanish) can be an alternative. The research done for the last few years has proven that, besides these ISCI systems, the joint use of an insulin pump and a continuous glucose monitoring system (MCG, in Spanish), can be useful for selected patients in order to improve the control of the glycaemia levels."
However, the existing systems do not automatically make decisions, and they always require that the patient interprets the glucose number and decides what to do at any given time with respect to the dose of insulin they have to administer.
Recently, with the aim of improving the control of this disease, the DT1 patient conditions and their quality of life, different initiatives to automate the glucose monitoring and the insulin dosage have started. The closed-loop system, commonly known as artificial pancreas (PA, in Spanish), is a system that incorporates a smart control algorithm (controller), that interprets the results about the glucose provided by a glucose sensor and decides the quantity of insulin which must be automatically administered at any time.
In this context, one of the main problems these PA systems have to face is the control of the glucose numbers after meals, as they must avoid an excessive infusion of insulin, which can cause hypoglycaemia. Besides this, the PA must regulate the infusion of insulin during the night, where different equipment has already proven its efficiency.
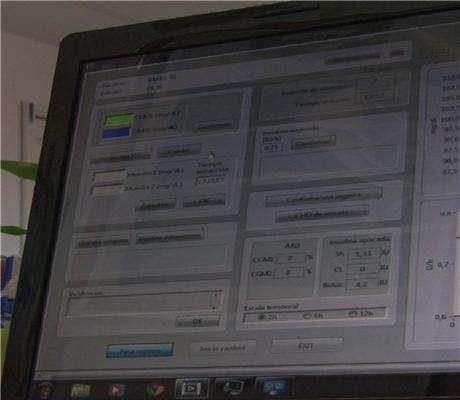
This trial intends to test the efficiency of an automatic controller with an original design for the adjustment of glucose levels after meals. The controller interprets the glucose results provided by a glucose sensor and decides, every 15 minutes, the quantity of insulin that must be administered automatically. "By controlling the glucose levels in the blood in a such effective way, we could reduce the health problems related to persistent hypoglycaemia," says the Dr. Ampudia-Blasco.
20 patients with type 1 diabetes are to take part in the study with an ISCI treatment: ten from the Hospital Clínico Universitario de Valencia and ten from the Hospital Clinic de Barcelona. The first study was done last week with one patient at the Clínico de Valencia.
According to the Dr. Juan F. Ascaso, Head of the Endocrinology and Nutrition Department of the Hospital Clínico Universitario de Valencia, "the artificial pancreas should give the patients autonomy and safety, allowing them to live with the disease without obsession. Besides that, it must avoid the complications caused when glucose levels fall. It consists of an approach to custom-designed treatments for each patient which reduce the problems caused by the treatments and costs."
According to the General Manager of the INCLIVA, Dr. Rafael Carmena, "this research brings a message of hope to diabetic patients. The development of an artificial pancreas system can improve, in the near future, the control of type 1 diabetes, the patients' conditions, and their quality of life. When the technology has been perfected, it will remove the necessity of manually injecting insulin and guarantee the administration of exact doses every time."
About Diabetes
Chronic hypoglycaemia, even in absence of symptoms, implies damage to multiple tissues, especially in the small retinal vessels, kidneys and peripheral nerves. That is why diabetes is one of the main causes of blindness, amputation and terminal kidney disease in developed societies.
In addition, diabetes implies an important risk of heart disease (ECV, in Spanish), as much for itself as for its relation to other risk factors, such as high blood pressure or dyslipidemia.
In the world, there are more than 347 million people with diabetes. In the Comunitat Valenciana, 14% of the population is affected.
Diabetes is increasing the burden of disease all over the world, particularly in developing countries. Causes are complex, but they are mostly related to a quick increase in weight, obesity and physical inactivity. The WHO expects diabetes to become the seventh leading cause of death worldwide in 2030 and calculates that the deaths from diabetes will increase by more than 50% in the next 10 years.
Two big types of diabetes exist. Type 1 diabetes, in which the body does not produce insulin, and type 2 diabetes, the most common, in which the body does not efficiently use the insulin.
Type 1 is a chronic disease that consists of selective destruction of the cells responsible for insulin production. After an asymptomatic period, when the pancreas cell destruction is complete and the clinical diagnosis is done, the disease requires insulin administration for life.
















