Brain circuit problem likely sets stage for the 'voices' that are symptom of schizophrenia
St. Jude Children's Research Hospital scientists have identified problems in a connection between brain structures that may predispose individuals to hearing the "voices" that are a common symptom of schizophrenia. The work appears in the June 6 issue of the journal Science.
Researchers linked the problem to a gene deletion. This leads to changes in brain chemistry that reduce the flow of information between two brain structures involved in processing auditory information.
The research marks the first time that a specific circuit in the brain has been linked to the auditory hallucinations, delusions and other psychotic symptoms of schizophrenia. The disease is a chronic, devastating brain disorder that affects about 1 percent of Americans and causes them to struggle with a variety of problems, including thinking, learning and memory.
The disrupted circuit identified in this study solves the mystery of how current antipsychotic drugs ease symptoms and provides a new focus for efforts to develop medications that quiet "voices" but cause fewer side effects.
"We think that reducing the flow of information between these two brain structures that play a central role in processing auditory information sets the stage for stress or other factors to come along and trigger the 'voices' that are the most common psychotic symptom of schizophrenia," said the study's corresponding author Stanislav Zakharenko, M.D., Ph.D., an associate member of the St. Jude Department of Developmental Neurobiology. "These findings also integrate several competing models regarding changes in the brain that lead to this complex disorder."
The work was done in a mouse model of the human genetic disorder 22q11 deletion syndrome. The syndrome occurs when part of chromosome 22 is deleted and individuals are left with one rather than the usual two copies of about 25 genes. About 30 percent of individuals with the deletion syndrome develop schizophrenia, making it one of the strongest risk factors for the disorder. DNA is the blueprint for life. Human DNA is organized into 23 pairs of chromosomes that are found in nearly every cell.
Earlier work from Zakharenko's laboratory linked one of the lost genes, Dgcr8, to brain changes in mice with the deletion syndrome that affect a structure important for learning and memory. They found evidence that the same mechanism was at work in patients with schizophrenia. Dgcr8 carries instructions for making small molecules called microRNAs that help regulate production of different proteins.
For this study, researchers used state-of-the-art tools to link the loss of Dgcr8 to changes that affect a different brain structure, the auditory thalamus. For decades antipsychotic drugs have been known to work by binding to a protein named the D2 dopamine receptor (Drd2). The binding blocks activity of the chemical messenger dopamine. Until now, however, how that quieted the "voices" of schizophrenia was unclear.
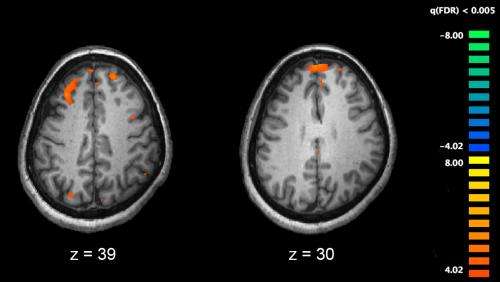
Working in mice with and without the 22q11 deletion, researchers showed that the strength of the nerve impulse from neurons in the auditory thalamus was reduced in mice with the deletion compared to normal mice. Electrical activity in other brain regions was not different.
Investigators showed that Drd2 levels were elevated in the auditory thalamus of mice with the deletion, but not in other brain regions. When researchers checked Drd2 levels in tissue from the same structure collected from 26 individuals with and without schizophrenia, scientists reported that protein levels were higher in patients with the disease.
As further evidence of Drd2's role in disrupting signals from the auditory thalamus, researchers tested neurons in the laboratory from different brain regions of mutant and normal mice by adding antipsychotic drugs haloperidol and clozapine. Those drugs work by targeting Drd2. Originally nerve impulses in the mutant neurons were reduced compared to normal mice. But the nerve impulses were almost universally enhanced by antipsychotics in neurons from mutant mice, but only in neurons from the auditory thalamus.
When researchers looked more closely at the missing 22q11 genes, they found that mice that lacked the Dgcr8 responded to a loud noise in a similar manner as schizophrenia patients. Treatment with haloperidol restored the normal startle response in the mice, just as the drug does in patients.
Studying schizophrenia and other brain disorders advances understanding of normal brain development and the missteps that lead to various catastrophic diseases, including pediatric brain tumors and other problems.
More information: "Specific disruption of thalamic inputs to the auditory cortex in schizophrenia models," by S. Chun et al. Science, 2014. www.sciencemag.org/lookup/doi/ … 1126/science.1253895



















