Development of new blood vessels not essential to growth of lymph node metastases
While the use of antiangiogenesis drugs that block the growth of new blood vessels can improve the treatment of some cancers, clinical trials of their ability to prevent the development of new metastases have failed. Now a study from the Massachusetts General Hospital (MGH) Cancer Center may have found at least one reason why. In their paper published online in the Journal of the National Cancer Institute, an MGH research team reports finding that the growth of metastases in lymph nodes—the most common site of cancer spread—does not require new blood vessels but instead takes advantage of existing blood vessels.
"We had previously shown that antiangiogenesis therapies were ineffective in animal models of lymphatic metastasis, but there was no data to explain the mechanism behind those observations," says Timothy Padera, Ph.D., of the Steele Laboratory of Tumor Biology in the MGH Department of Radiation Oncology, senior author of the paper. "Using a novel model we developed to facilitate discoveries about the growth and spread of lymph node metastases, we show that angiogenesis does not occur in lymph node metastases, providing a mechanism for resistance to angiogenic therapy in these situations."
For most types of solid tumors, the presence of lymph node metastases indicates a poorer prognosis and the need for chemotherapy or other systemic treatments that are delivered throughout the body. But the actual role of lymph node metastases in the spread of cancer has been controversial, Padera notes. Some experts believe that it signifies the inherent ability of the primary tumor to spread. Other investigators believe that lymph node metastasis is an essential part of the process leading to metastases in other parts of the body and that metastatic cells in the lymph nodes pass into the bloodstream and seed the growth of new tumors.
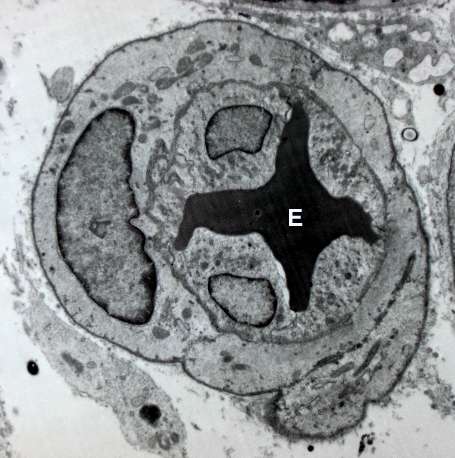
To follow up their previous findings that antiangiogenesis therapies could not stop the development or growth of lymph node metastases, the MGH team designed the current study. Using a mouse model of cancer that provides direct microscopic access to lymph nodes, they first found that the initiation and growth of node metastases did not involve the development of new blood vessels. They also found no increase in the levels of angiogenesis-inducing factors or in the expression of angiogenesis-related genes in metastatic lymph nodes. In fact, levels of two antiangiogenesis factors were elevated. Analysis of metastatic lymph nodes from human patients with colon or head and neck cancers also revealed no evidence of angiogenesis.
In the mouse model, treating node metastases with two angiogenesis inhibitors that have different mechanisms of action did not change the density of blood vessels or the growth of the metastases. Finally, comparing lymph node metastases from rectal cancer patients who had been treated with the angiogenesis inhibitor bevacizumab with those from patients that received no antiangiogenesis therapy found no difference in blood vessel density within the metastatic nodes. The researchers also found that lymph node metastases appear to have developed from several different tumor cells that lodged in the nodes, not from a single tumor cell as is the case with many but not all distant metastases.
"The primary implication of our findings is that, since lymph node metastases do not require the development of new blood vessels, antiangiogenic therapy will not inhibit lymphatic metastasis. Other therapies need to be tested for the treatment of patients at risk for lymph node metastasis," says Padera, who is an assistant professor of radiation oncology at Harvard Medical School. "Now we need to answer the question of whether or not lymph node metastases actually can seed distant metastases, which would indicate how aggressively they need to be treated."















