Prion trials and tribulations: Finding the right tools and experimental models
Prions are fascinating, enigmatic, and might teach us not only about rare prion diseases like Creutzfeld-Jakob disease, mad cow disease, or scrapie, but also about other more common neurodgenerative diseases. Two studies published on July 2nd in PLOS Pathogens report progress with novel tools and paradigms to study prion disease.
Several research groups have recently succeeded in generating infectious prions with prion protein produced by bacteria in test tubes under consistent and controlled conditions. Such synthetic prions are a critical tool to study how prions cause disease in general and to test the "protein-only" hypothesis, which states that the mutant prion protein itself can trigger the disease by co-opting other prion proteins to form aggregates that are toxic to nerve cells. Jiyan Ma, from the Van Andel Research Institute in Grand Rapids, USA, and colleagues tested whether the properties of synthetically generated prions are the same as those of natural disease-causing prions, and whether the disease caused by synthetic prions is identical to naturally occurring prion disease.
They demonstrate that similar to the classical disease-causing prions, synthetic prions are infectious in a concentration-dependent way, and are able to cause prion disease in normal mice not only by direct injection into the brain (which is the easiest but not a naturally occurring way of prion transmission) but also by other routes. The researchers also show that the synthetic prions induced pathological changes typical for classic prion disease, including the dissemination of disease-specific prion protein accumulation and the route and mechanism of invasion of nerve cells in the brain. They conclude that their results "demonstrate the similarity of synthetically generated prion to the infectious agent in TSEs [transmissible spongiform encephalopathies, another term for prion diseases] and provide strong supporting evidence for the prion hypothesis."
About 15% of human prion disease is heritable and caused by dominant mutations in the human PRP gene. The mutations are thought to predispose the resulting PRP protein proteins to adapt the disease conformation and trigger the cascade that kills nerve cells. Much of the study of inherited human prion disease in mice has focused on mixing mutant human prions—isolated from human patients or produced by transgenic mice carrying the mutant human gene—with normal mouse prions in order to establish whether the mutant human prions are infectious, i.e. whether they can change normal proteins to the disease-associated conformation (or shape).
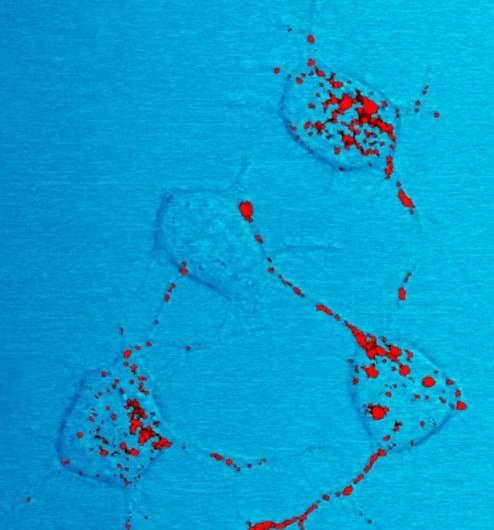
John Collinge, from University College London, UK, and colleagues answered a crucial question regarding such studies, namely whether superimposition of pathogenic human PrP mutation into mouse PrP (which is similar but not identical) will have the same structural consequences as occur in the human brain. They focused on a specific mutation underlying an inherited form of human prion disease called Gerstmann-Sträussler-Scheinker (GSS) disease. This mutation causes an amino-acid substitution (proline-to-leucine) in the prion protein, human PrP 102L for short. In the brain of patients with GSS disease, this mutant prion (GSS-102L) co-exists with a heterogeneous mixture of normal PrP and other PrP derivatives, which it somehow manages to co-opt into forming aggregates that are toxic to the nerve cells.
To characterize the transmission capabilities of the GSS-associated prions, the researchers tested whether the ability of GSS P102L to cause prion disease in mice depended on what other types of prion proteins and derivatives were present. They examined whether GSS P102L prions could infect transgenic mice that express human mutant 102L PrP, human normal PrP, or normal mouse PrP. Injecting a pure preparation of GSS P102L prions into the brains of the three different types of mice, they found that GSS P102L prions can only infect transgenic mice expressing human 102L PrP, i.e. those carrying the identical mutant human gene. Mice expressing normal human PrP or normal mouse PrP were completely resistant to infection with GSS-102L prions.
"Collectively", the researchers say, their data "establish that GSS-102L prions which replicate with high efficiency in a host expressing human PrP 102L are unable to propagate using wild-type [normal] human PrP or wild-type mouse PrP as substrate." These results differ from the reported transmission properties of prions generated in GSS-P102L challenged mice expressing mouse PrP 101L (the equivalent mutation in the closely related but not identical mouse PrP): such prions readily infect animals expressing normal human or normal mouse PrP. Commenting on the discrepancy, the researchers suggest that the superimposition of the human on the mouse mutation might have generated experimental prion strains with different transmission characteristics from those of authentic human prion strains. Overall, they conclude that "future transgenic modeling of infectious prion diseases should focus exclusively on expression of mutant human PrP, as other approaches may generate novel experimental prion strains that are unrelated to human disease."
Better tools and better paradigms to study prion diseases should help the understanding of how these diseases spread and devastate mammalian brains, and eventually lead to efficient treatment and prevention strategies.
More information:
PLOS Pathogens: dx.plos.org/10.1371/journal.ppat.1004958
PLOS Pathogens: dx.plos.org/10.1371/journal.ppat.1004953
















