Researcher discusses state of the immunotherapy field
After decades in the shadows, treatments that encourage a patient's own immune system to target their cancer – known as immunotherapy – have emerged as one of the brightest hopes in cancer research, and have rarely been out of the headlines in recent months.
Our chief clinician, Professor Peter Johnson, has worked in this field for several decades, witnessing early frustrations finally transform into clinical success, and even potential cures.
We caught up with him to get his views on the progress to date, where the field is heading, and the challenges facing researchers and doctors as immunotherapy becomes mainstream.
How have things changed since you started working in immunotherapy research?
The immune system's potential to treat cancer has been known for over a century. But even when I started out in the 1990s, our ability to apply this to help patients was still very much in its infancy.
One of our first approaches was to inject patients with molecules called cytokines, to try to stimulate their immune system into action. Then we tried to use engineered viruses to modify tumours to produce their own cytokines, to get the immune system's attention.
We also tried using antibodies to target the tumour directly – this was successful for lymphoma, but not so much for other cancer types, so we tried attaching a 'payload' to the antibodies – toxins or radioactive particles.
Another approach taken by many labs was essentially a form of therapeutic vaccination. We were trying to wake up patients' immune systems with different molecules, generally derived from proteins we knew to be over-produced by certain types of cancer. Quite a lot of the work over the 90s can be broadly summed up as different types of vaccination – and most of it didn't really work.
Most recently, we began to focus on antibodies aimed at the immune system's control switches, rather than the cancer itself. And we started working on the first one of those, which was a stimulating antibody, in the late 1990s and took that through into a phase 1 trial.
But it was only when we saw the results of clinical trials of drugs that target a particular molecular switch on immune cells, called CTLA-4, that we saw really striking results. And that's what's been catalysing the field as a whole.
What we know now is that the body keeps its immune system on a very tight leash. And until it's specifically unleashed – in this case with a drug – it's hard to get it to do anything against our own cells, which of course includes cancer. And this explains why many earlier approaches failed.
Why did it take so long to find this out?
At the beginning of the 2000s, the cancer research field was broadly divided. On the one hand you had 'genome' people, who were studying cancer's DNA and trying to target specific faults with drugs like imatinib, with considerable success in some cases.
And then there were the immunologists. We were in the minority, and regarded as slightly misguided, on the grounds that the immune system was a hugely complicated, fine-tuned system. Many people thought we were never going to find a way to reprogram it in a predictable manner.
And this was reinforced by a lot of the work that had gone on with vaccine therapy. Patients were vaccinated with all sorts of molecules – peptides, nucleic acid – with entire tumour cells, with special immune cells loaded with parts of tumour cells, or fused with tumour cells… you name it, we tried vaccinating with it.
But what became clear was that this approach on its own just wasn't going to work – in 2004, a group of researchers at the US National Cancer Institute, led by Steven Rosenberg, wrote a thoughtful piece in Nature Medicine, essentially saying that cancer vaccines had failed.
We were all quite upset about it at the time, but it was probably a fair comment.
What kept you going?
The thing was, we always saw a few dramatic responses.
So even in the early days, when we treated people with high doses of cytokines, there would always be a few people alive and well a few years later who'd had a good response – and this was something we only saw rarely with conventional chemotherapy. It was always a hallmark of immunotherapy. Whether it was a cytokine or a complicated cellular vaccine, there were always a few people who did better than you'd expect. Enough to keep us plugging on.
What was the moment you first thought, 'hang on, this is actually going to work'?
It really only was when we saw the responses of patients with melanoma given a drug that targets CTLA-4 [now known as ipilimumab (Yervoy)] that people started to think that it might work. The real turning point was the trial published in the New England Journal of Medicine in 2010, where we started to see dramatic responses in a substantial minority of patients. Most cancer doctors work along pretty simple lines: you treat your patients and if the tumour really shrinks you think 'this is good'!
Now we've got a few new drugs – collectively called checkpoint blockers – that are rapidly coming through the system for melanoma, lung cancer, and several other cancers. And there are more in the pipeline.
Why have these cancers been the focus of so much of the recent work?
This is for three reasons.
First, because these cancers, especially kidney cancer and melanoma, seem to be able to lie dormant for a long time – you remove patients' primary tumours but then the disease can come back years later. Where have those cancer cells been all that time? They must have been around, but being held at bay by the immune system. So this was a big clue.
The next clue was spontaneous remission – people who get better despite having not had active treatment – and these seem to be more common in people with melanoma and kidney cancers.
The third is the more recent knowledge that you can find immune cells in the circulation of people with melanoma that can recognise molecules on their tumour.
So there were bits of circumstantial evidence, but it was only that.
And then the other reason, of course, is the fact that for many patients with these cancers, conventional treatments – chemotherapy and radiotherapy – were largely ineffective. These were patients who really needed something new.
On the flipside, are there cancer types where you suspect immunotherapy will be less effective?
It seems that the genetically more 'scrambled' tumours respond better, so it's looking likely that the cancer types that tend to have fewer genetic faults – children's cancers, certain types of brain tumour – may be difficult to treat with immunotherapy.
There are some other cancers where we are still not sure, such as prostate and breast cancer.
What about side-effects?
The principal problem with immunotherapy is that the immune system can attack a patient's own tissues – an 'autoimmune' response. During the early days of cancer immunotherapy, when nothing seemed to work, critics would say to us, "…and another thing – you will get autoimmunity". To which our response was always, "we'll worry about that when it happens" – if we get autoimmunity we'll know something is working.
But with these new drugs, it has happened, because they are working. In a proportion of cases, we see two important things: pneumonitis, where the immune system attacks the lungs, or colitis in the bowels. There are also less common side effects, for example skin rashes, or where the pituitary or thyroid glands are affected, so that's manageable because you can replace the hormones they produce, provided you make the diagnosis quickly.
And as time has gone on we've got much better at anticipating and managing side effects, so now if we see autoimmunity starting up we give steroids very quickly, to switch it off, and we know that we've got other treatments in reserve if the steroids aren't enough.
There's been a lot of enthusiastic coverage of these new drugs. Can we use the word 'cure' yet?
I think it's legitimate to say that, if someone with very advanced melanoma had a treatment a decade ago, and there's still no sign of it, then there's a reasonable chance they may be cured. And this is the case for one in five people who took part in the early ipilimumab studies.
With the combinations of ipilimumab and the newer checkpoint drugs, which target a molecule called PD1, it's a bit too early to say – the trials haven't been followed up for long enough yet, but the early indications are very promising.
What do we know about who to give these drugs to? And how's this view evolving?
This is an area of intense research, and it's a moving target. There's a bit of evidence that if certain molecules are present in high levels on either a patient's tumour cells, or their immune cells, then this can help predict who will respond. But this isn't perfect – we see responses in people who don't have these molecules, and there are also people who do have them, but who aren't responding.
Personally, I think the key to understanding all this will be unravelling how three things interact: first, the genes that are faulty and activated in the tumour itself; second, the molecules released by the cells into the tumour's immediate environment; and third, the state of activation of immune cells in and around the tumour. It's basically a three-way Mexican stand-off between these three things, and we need to understand what's going on.
Fortunately the latest technology is allowing us to do that, and things are really progressing quickly.
What about cost of these drugs? Can the NHS afford them?
Despite some of the headlines, I'm actually more optimistic about the cost of these antibodies than I am about some new cancer treatments we see. Because the actual process of making them is not especially complex – our PhD students can learn how to make a new antibody in a couple of months.
On top of this, there's such competition in the market now – at least half a dozen huge Pharma companies are doing clinical trials, competing with each other, so that must drive the price down.
The NHS recently struck a deal to make the second of these new drugs, pembrolizumab, available at an acceptable price – so there may be less to worry about than initially seemed to be the case.
Aside from checkpoint-blocking drugs, what else has caught your eye?
What I think we'll see increasingly is the idea of personalised vaccine therapy. The reason that we haven't made faster progress in immunotherapy is that we didn't know how to 'take the brakes off', which we can now do – to a degree – with checkpoint drugs.
And in a way, the recent combination antibody trials, using two different checkpoint-blocking drugs, are a demonstration of why we need to do this: more patients respond – better than either drug on its own – but more of them get serious side effects. What we really need to do is to put some specificity into how we stimulate the immune system – to really target it at the tumour, as well as releasing the breaks.
But if you combine a vaccine with checkpoint drugs, you suddenly have a whole different set of questions you can ask about how the immune system is responding, and a whole different way of stimulating an immune response. This has to be the way forward.
How do they work and how do you make them?
In theory, first, you can analyse the genes in a patient's tumour, see what's mutated, and run that information through computer software that tells you which faulty proteins the tumour's making and which parts of them are likely to attract the immune system.
Then, you could chemically manufacture short fragments of these particular proteins and give them to the patient alongside a checkpoint-blocking drug.
But there are challenges. There are engineering problems in scaling the whole process up, but there is also the problem of how to work out the best vaccine from the DNA sequence. The software we have at the moment is far from perfect. So there's going to be a lot of software development, analysis and experimentation before we're really confident it works as it should.
What do you make of the 'engineered' T-cell treatments that have garnered a fair few headlines recently?
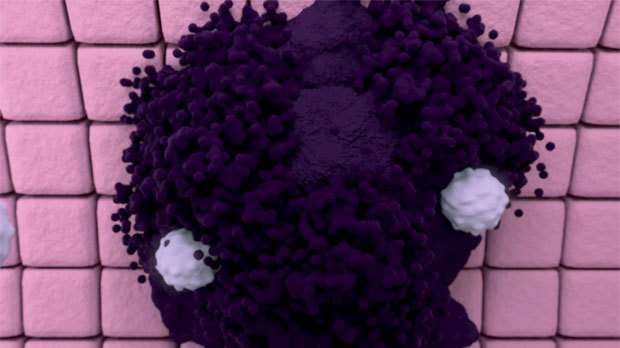
Another thing on the horizon is the whole field of engineered T-cells, also known as 'chimeric antigen receptor' (CAR) T- cells – where you create immune cells that are precision engineered to target and destroy cancer cells that bear particular proteins on their surface. So far these treatments look most promising in particular blood cancers – B cell leukaemia, and lymphoma.
Growing these cells is a complicated process and resource intensive, but a number of pharma companies are investing in the technology to try and bring them into wider clinical testing.
Because this approach is so powerful, the other issue with using it more widely is that the treatment can wipe out any cells that carry the particular target protein – for B cell leukaemia or lymphoma, this means removing all a person's normal B cells too, so they can no longer produce their own antibodies. You can live without B cells, but you are dependent on having antibody replacement treatments for the rest of your life.
Applying the same approach for solid tumours is trickier, and there have been some real problems in some of the trials with the drugs attacking the liver. Your B cells are important, but they're not totally essential, whereas having a liver is.
What's your immunotherapy 'Grand Challenge'? If you could solve one big problem, what would it be?
I think it would be a system to understand, at a given moment, in a given patient, what their immune system is doing. At the moment we have limited information on what the true effects of immunotherapy are, we don't have good ways to predict how a patient is responding – the molecules we measure in the blood seem to be quite unhelpful.
So I would really like some ready means of both predicting response and measuring outcome, in terms of what the immune system is doing, because only by doing that we can start adjusting the way we do it quickly.
This brings us back to the old problem of 'measuring immunity', which is something we've always struggled with since the early days. But if we can crack that, then we can really use these treatments in the ideal way, and work out how to do the best for our patients.
More information: "Cancer immunotherapy: moving beyond current vaccines." Nature Medicine 10, 909 - 915 (2004) DOI: 10.1038/nm1100
"Clinical and biological effects of an agonist anti-CD40 antibody: a Cancer Research UK phase I study." Clin Cancer Res. 2015 Mar 15;21(6):1321-8. DOI: 10.1158/1078-0432.CCR-14-2355
"Improved survival with ipilimumab in patients with metastatic melanoma." N Engl J Med. 2010 Aug 19;363(8):711-23. DOI: 10.1056/NEJMoa1003466
















