Cells carry 'memory' of injury, which could reveal why chronic pain persists
A new study from King's College London offers clues as to why chronic pain can persist, even when the injury that caused it has gone. Although still in its infancy, this research could explain how small and seemingly innocuous injuries leave molecular 'footprints' which add up to more lasting damage, and ultimately chronic pain.
All of us are likely to know someone who suffers from persistent pain - it is a very common condition, which can be caused by sports injuries, various diseases and the process of ageing. Treatment options are limited and doctors are often unable to offer anything more than partial relief with painkillers, leaving their patients resigned to suffering.
While chronic pain can have many different causes, the outcome is often the same: an overly sensitive nervous system which responds much more than it normally would. However, a question still remains as to why the nervous system should remain in this sensitive state over long periods of time, especially in instances where the underlying injury or disease has gone.
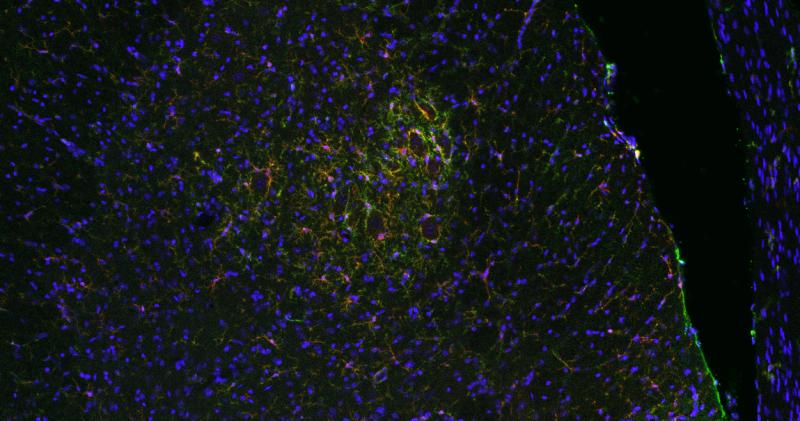
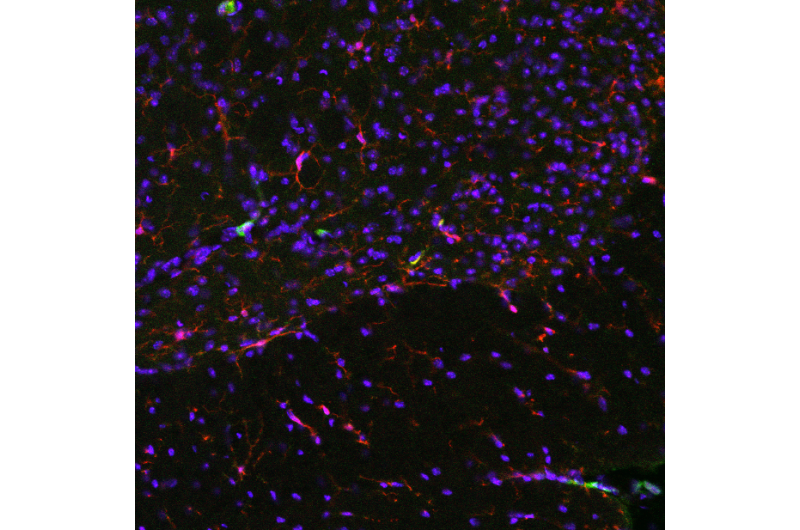
Researchers from King's sought to answer this question by examining immune cells in the nervous system of mice, which are known to be important for the generation of persistent pain.
In the study, published today in Cell Reports, they found that nerve damage changes epigenetic marks on some of the genes in these immune cells. Epigenetics is the process that determines which gene is expressed and where. Some epigenetic signals have direct functional consequences, while others are just primers: flags that indicate a potential to act or be modified.
The cells examined in this King's study still behaved as normal, but the existence of these novel epigenetic marks may mean that they carry a 'memory' of the initial injury.
Dr Franziska Denk, first author of the study, from the Wolfson Centre for Age Related Diseases at the Institute of Psychiatry, Psychology & Neuroscience (IoPPN), King's College London, said: 'We are ultimately trying to reveal why pain can turn into a chronic condition. We already knew that chronic pain patients have nerves that are more active, and we think this is probably due to various proteins and channels in those nerves having different properties.
However, it is unclear why these nerves should remain in this overactive, highly sensitive state, even when the initial injury or disease has gone: the back pain from two years ago that never quite went away or the joints that are still painful despite your rheumatoid arthritis being in remission.'
Dr Denk added: 'We want to know why these proteins and channels should maintain their altered function over such a long period of time. Cells have housekeeping systems by which the majority of their content are replaced and renewed every few weeks and months - so why do crucial proteins keep being replaced by malfunctioning versions of themselves? Our study is the very first step towards trying to answer this question by exploring the possibility that changes in chronic pain may persist because of epigenetics. We hope that future research in this area could help in the search for novel therapeutic targets.'
Professor Stephen McMahon from the IoPPN at King's College London said: 'This research raises many interesting questions: do neurons also acquire epigenetic footprints as a result of nerve injury? Do these molecular footprints affect the function of proteins? And are they ultimately the reason that chronic pain persists in patients over such long periods of time?
'The last question is particularly hard to answer, because to study epigenetics we need access to pure cell populations. Obviously, many of these are only accessible in postmortem tissue. However, colleagues at King's are already doing this in psychiatry, through studies such as the The PsychENCODE project, so it is possible.'
Dr Giovanna Lalli, Neuroscience & Mental Health Senior Portfolio Developer at the Wellcome Trust, which part-funded the study, said: 'People develop chronic pain for a huge variety of reasons. We therefore need an equally diverse range of treatments to tackle the different root causes.
'The clues from this study, suggesting epigenetic changes may be involved in pain persisting, will hopefully lead us to better understand the mechanisms underlying chronic pain.'

















