June 10, 2016 report
New liquid biopsy techniques at the bleeding edge of cancer
(Medical Xpress)—There's many buzzwords being thrown around in medicine these days. In cancer treatment, blanket terms like "precision medicine" and "immunotherapy" hint at the promise of a rapidly changing technology base, but at the same time, can invariably leave both patients and caregivers alike a bit foggy on a precise meaning of the terms. An emerging diagnostic technique of similar broad scope that is having a clear impact right now in cancer is the "liquid biopsy".
Essentially, it involves taking material from patient's blood, CSF, urine or other fluids, and analyzing it for tumor marker genes or metabolites. It's not really designed to supplant the direct solid tumor biopsy that is critical to the initial pathological diagnosis of cancer. The information you get in looking at the 'in situ' form and arrangement of tumor cells in a histological sample is simply irreplaceable. But what the liquid biopsy can now do extremely well is provide up to date 'meeting minutes' for the subsequent treatment of that cancer.
Tumors do not take chemotherapy sitting down. They predictably arm themselves through a succession of genetic and metabolic pivots in which they acquire resistance to the drugs. Generally this involves upregulating enzymes which pump out and modify drugs so the body can excrete them. Because of this, new immunotherapies based on stimulating the patient's own immune system may offer a better approach than any particular drug cocktail. Instead of antimitotic or cytotoxic drugs, man-made immuno proteins which enhance endogenous antitumor responses are given.
Sitting right at the nexus of these new technologies is a company called Biocept. They just launched their groundbreaking 'liquid biopsy immuno-oncology PD-L1 test'. PD-L1 stands for Programmed Cell Death Ligand 1 which, perhaps not surprisingly, binds to a protein found on T cells and pro-B cells known as Programmed Cell Death Protein 1. When this happens, activation of T cells is blocked and the immune system is toned down. This normally acts as an important checkpoint which keeps an overzealous immune system from attacking the body's own healthy tissues. However, all bets are off in cancer where you want all the immune action you can muster.
Patients with cancers expressing PD-L1 have been found to respond well to immunotherapy. Drugs like pembrolizumab, that target its PD-1 receptor, have gotten FDA approval for certain cancers like advanced non-small cell lung cancer. To get cutting edge drugs like these patients frequently need to be qualified under the auspices of a formal drug trial. Biocept's blood-based PD-L1 expression test can readily provide that validation.
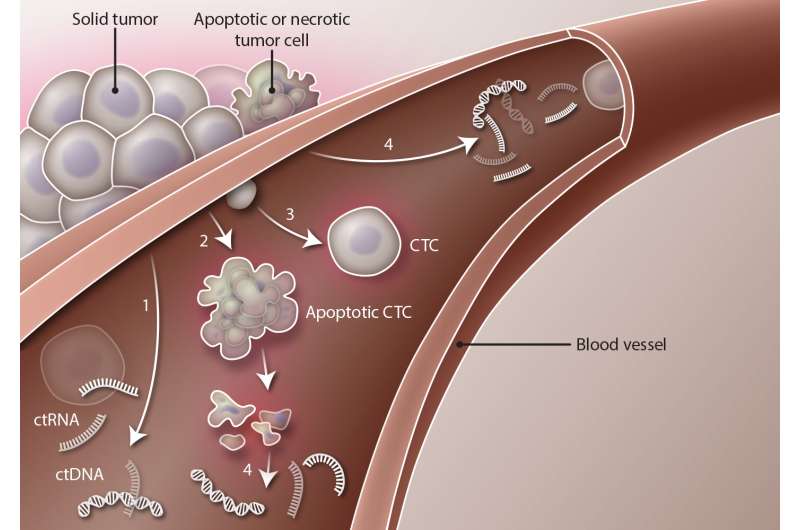
I spoke recently with Biocept's Veena Singh who described the technology behind several of their new diagnostic tests. They now have the ability to isolate single cancer cells from a sample using microfluidics. Using fluorescent labels they can eliminate healthy cells from the pool, and quantify PD-L1 expression levels directly in the circulating tumor cells (CTCs). These rouge, potentially metastatic cells from the primary tumor, are generally rare—perhaps just a handful in a 10ml sample. By contrast, in a 'liquid tumor' a direct hematologic cancer (like leukemia or lymphoma), they would be more abundant.
In addition to CTCs, Biocept can also analyze cell-free or circulating tumor (ct)DNA. This source might be up 100 times more abundant in the blood—perhaps hundreds of what we might call 'genome equivalents' of a CTC. With a handy blood source, PD-L1 levels can be readily monitored throughout the course of therapy. This is a welcome development for any patient for whom the word 'biopsy' quite reasonably elicits considerable angst.
Considering that a typical bone biopsy for the above mentioned liquid tumors involves a somewhat nasty dual sample technique (excising a lamprey-like solid core of bone and aspirating some liquid marrow), less invasive methods are highly sought. The same sentiment applies for spinal tap biopsy of tumors spreading the central nervous system. In non small cell long cancer, brain metastases and leptomengial disease are common sequelae. Biocept can now analyze the CSF in such cases to determine if tumor cells or DNA (which may not pass readily into general circulation), is there.
The number of potential tumor markers that can be analyzed is exploding. Additionally, other pathogenic alterations like single nucleotide variants, (SNVs) copy number variants (CNVs), fusions, rearrangements, and insertions or deletions can be quantified. At this week's ASCO cancer meeting in Chicago (where Biocept had several new abstracts), Vice President Joe Biden spoke to much the optimism now palpable in the business.
Now perhaps on equal footing with the massive proliferation of genetic minutia in the understanding of cancer is a parallel appreciation of the what makes cancer tick at the level of basic metabolism. For example, in the above mentioned case for the activation of T cells in immunity, it is now understood that a metabolic reprogramming from oxidative energy generation to glycolysis is required. This mimics much of what is known regarding both normal developmental protocol (as in embryogenesis), and also in tumorigenesis under the commonly known Warburg effect.
What is nothing short of revelatory, is have reached a critical mass where we can now explain these metabolic transformations in light of their direct control by new tumor markers nearly as fast as these markers can be discovered. For example, it was recently found that when PD1 is ligated in T cells that have been activated, they are not able to fully engage in glycolysis to generate the full amino acid economy they need to function. Instead they switch a metabolism of fatty acid β-oxidation and lipolysis. While admittedly complex, such observations point to a mechanistic explanation of T-cell function and their capacity to be invigorated by PD-1 blockade.
More information: ir.biocept.com/releasedetail.cfm?ReleaseID=973345
© 2016 Medical Xpress



















