Using epigenetics to help the immune system fight ovarian cancer
Sometimes, even a miracle needs a hand.
Immunotherapy, a cancer treatment approach that's decades old, has become the hottest subject in oncology. In the past few years, researchers have developed a host of new drugs capable of jumpstarting the immune response to tumors. Now, these treatments have reached the clinic. Reports on their success were the focus of numerous presentations at this summer's American Society for Clinical Oncology (ASCO) conference in Chicago. In naming immunotherapy its Advance of the Year for 2016, ASCO President Julie Vose, M.D., said "no recent advance has been more transformative." In media reports, other physicians have said immunotherapy could be "an even more important intervention than chemotherapy," and patients have chronicled "miracle" results.
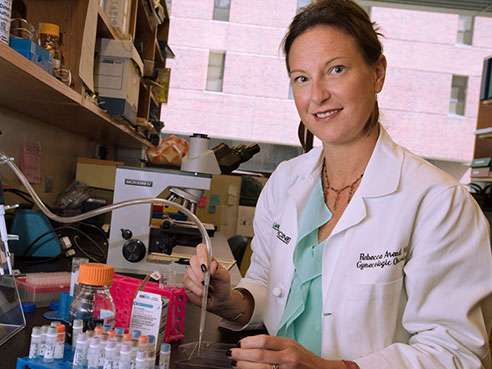
"Cancer patients who respond to immunotherapy tend to have a prolonged response," says Rebecca C. Arend, M.D., an assistant professor in the UAB Division of Gynecologic Oncology and associate scientist in the Experimental Therapeutics Program at the UAB Comprehensive Cancer Center who specializes in treating ovarian cancer. "It's really exciting, because this is something that we don't usually see with chemotherapy and 75 percent of patients recur within two years of receiving initial chemotherapy and surgery for ovarian cancer." Unfortunately, only a fraction of patients benefit from immunotherapy treatments. So Arend, with a new grant from UAB's Center for Clinical and Translational Science, is exploring a fresh approach: "priming" the body to respond to immunotherapy using another new class of drugs: epigenetic modifiers.
A loophole in the body's defenses
There are many varieties of immunotherapy, including checkpoint inhibitors, CAR T cell therapy, therapeutic cancer vaccines and oncolytic viruses. But they all begin with the concept that the immune system is very good at isolating and destroying unhealthy cells. The trouble is, tumors often develop mutations that let them escape these attacks by switching off or otherwise thwarting the immune response. Immunotherapies work to get the body's defense system back into the fight.
The greatest excitement at the moment surrounds the new class of checkpoint inhibitors, including PD-1 and CTLA-4 inhibitors. "Your body has a natural response of putting the brakes on the immune system," says Arend. "These drugs take those brakes off."
Why is the immune system braking in the face of a grave threat like cancer? Some years ago, researchers realized that T cells, the immune system's frontline soldiers, are often found surrounding tumors. But instead of attacking the malignant cells, or calling in other troops, they aren't doing much of anything. That's because the tumor cells have co-opted the T cells' on-off switch. They have to have one: Without a "stop" sign, T cells would keep on attacking, chewing into healthy tissue and causing serious damage. So they have several different kinds of checkpoint receptors to receive "stand-down" messages from healthy cells in the area. But cancer cells know how to send these messages, too, blunting the immune response. The discovery of these checkpoints, and the development of drugs to block them, has brought immunotherapy to the fore in cancer care.
The most well-known of the checkpoint inhibitors, pembrolizumab (Keytruda), is a PD-1 inhibitor. It was initially approved by the FDA in 2014 to treat advanced melanoma, but it has been used successfully to treat several other cancers, including non-small cell lung cancer and head and neck cancer. Former President Jimmy Carter credited the drug with shrinking his brain tumors and saving his life. Other patients have experienced similarly striking results. But many more do not. In one study of a different checkpoint inhibitor, targeting CTLA–4, a fifth of patients with metastatic melanoma experienced durable remissions.
Mutations could hold the key
What's the difference between responders and non-responders? Recent studies have shown that a key factor could be the mutation burden of a patient's tumor. All cancers are triggered by mutations, but the number of mutations varies widely. "Mutation burden enhances the response to immunotherapy, probably because the tumor looks even more like non-self," says Arend. "So more and more research is being done to look at ways that we can prime tumors to look like the ones in these good responders."
Several human trials are already underway using epigenome-modifying drugs in combination with checkpoint inhibitors. There are several theories as to why the combination of epigenetic and immunotherapy drugs is more successful than either alone. "One theory is that epigenetic drugs enhance immune modulator pathways," Arend says. "Another is that you are causing more genomic disarray in the tumor itself. And there are papers that have shown that resistance to immunotherapy is because of epigenetic modification. So there could be multiple interactions."
Arend and others also suspect that the timing and dosage of the combination will be critical to success. "Most of the human trials that are ongoing basically give the drugs at the same time," Arend says. "I don't know that that's the way to go. It may be that you need to give the epigenetic drug first, followed by immunotherapy. And it may be more beneficial to give it upfront, rather than later on in the course of disease."
The right drug, for the right patient, at the right time
Arend hopes to gain new insight into these questions thanks to a Multidisciplinary Pilot Program Award from the UAB CCTS. With the award, one of nine given by the CCTS in 2016, Arend will study the immunotherapy/epigenetic drug combination in laboratory models of ovarian cancer, and in a potential human clinical trial. The Pilot Program grants offer up to $60,000 to cover one year of research into an emerging, high-potential problem.
Arend notes that she has been working under the mentorship of Cancer Center senior scientist Donald Buchsbaum, Ph.D., since her first year as a fellow at UAB. She is partially funded by a training scholarship through the American Board of Obstetrics and Gynecology (ABOG) Education Foundation. Her collaborators on this research include Troy Randall, Ph.D., J. Claude Bennett Professor of Medicine in the UAB Division of Clinical Immunology and Rheumatology, who is an expert in immune signaling in cancer; and Sara Cooper, Ph.D., investigator at Huntsville's HudsonAlpha Institute for Biotechnology, who is studying genomic profiling to predict drug response in ovarian cancer. (In 2014, the UAB Comprehensive Cancer Center and HudsonAlpha launched a consortium to combine research efforts at the institutions.) The research team will be studying two types of epigenetic drugs—DNA methyltransferase inhibitors and histone deacetylase inhibitors—in combination with an immunotherapy drug, a PD1 inhibitor.
In a separate project, Arend is collaborating with Cooper "to fine-tune the process of prescribing medications for ovarian cancer patients with specific genetic signatures," she says. Arend is also working with HudsonAlpha scientists to study the immune repertoire (subtypes of immune proteins) found in T cell receptors. "We're sequencing the RNA of T cell receptors as a possible marker of response to PD1 therapy," Arend says.
Personalized medicine is a major interest for Arend. "I'm a clinician-scientist," she says. "I give the chemotherapy and I also study new treatments in the lab. I want to understand which patients are going to respond to which drugs, and why."

















