New study shows targeted therapy needed for breast cancer with brain metastases
Researchers at the University of Pittsburgh Cancer Institute (UPCI) and Magee-Womens Research Institute (MWRI) have discovered molecular changes in the primary tumor of breast cancer patients who developed brain metastases. The finding is expected to lead to improved diagnosis and targeted therapies.
The results, to be published in the Journal of the American Medical Association (JAMA) Oncology and presented this week at the 2016 San Antonio Breast Cancer Symposium, indicate that patients' treatments should be tailored not only for the original breast cancer, but also the brain tumors, said Adrian Lee, Ph.D., director of the Institute for Precision Medicine, a joint effort by UPMC and the University of Pittsburgh, and director of the Women's Cancer Research Center, a collaboration between UPCI and MWRI.
"The brain is a common and catastrophic site of metastasis for breast cancer patients," said Lee. "Our study showed that despite the large degree of similarity between the initial breast tumor and the brain metastatic tumor, there were enough alterations to support comprehensive profiling of metastases to potentially alter the course of treatment."
There are many types of breast cancers, and about 20 percent of them are identified as HER2-positive, meaning the cancer cells have more of a protein called HER2 that causes the cells to grow faster than those with normal levels of the protein. These patients' cancers typically respond to targeted therapies. However, breast cancer patients with brain metastases who are identified as HER2-negative do not respond favorably to the same therapies.
Lee's research team set out to determine if there were molecular differences in the primary breast tumors and their patient-matched brain metastatic tumors that would enhance treatment options.
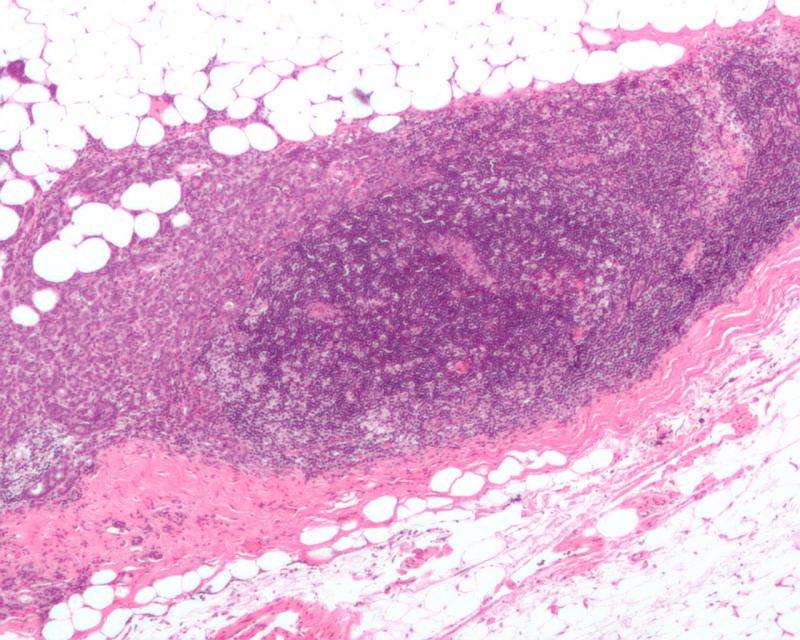
Little research is available because there are few opportunities to study primary breast tissue with their patient-matched brain metastases. The research team tested tumors from 20 patients from two academic institutions, the University of Pittsburgh and the Royal College of Surgeons in Ireland. Among the discoveries was that the primary tumor initially identified as HER2-negative actually switched to HER2-positive in the metastatic brain tumor.
"This now means we can screen for presence of HER2 so that we can change and target the therapy to improve outcomes for our patients," said Dr. Lee.
















