Study highlights possible Achilles' heel in key immune memory cells
The capacity for memory isn't exclusive to the brain. The immune system, with its sprawling network of diverse cell types, can recall the pathogens it meets, helping it to swiftly neutralize those intruders upon future encounters.
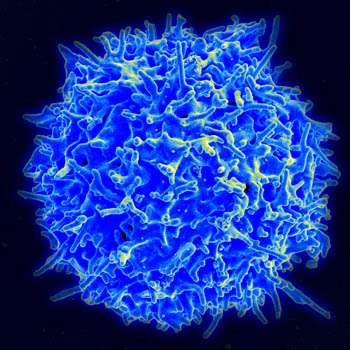
For the last several years, BWH's Thomas Kupper, MD, Chair of the Department of Dermatology, and his colleagues have been studying a unique kind of immune memory cell, known as a tissue-resident memory T (TRM) cell. Discovered more than 10 years ago by Rachael Clark, MD, PhD (also in BWH Dermatology), these cells live in peripheral tissues, like the skin, gut and joints, and are thought to be a key source of the immune system's protective memory. Although much remains to be learned about the biology of these specialized memory T-cells, dysfunctional TRM cells are strongly implicated in autoimmune diseases, such as psoriasis, rheumatoid arthritis, inflammatory bowel disease and other conditions.
To uncover the key genetic signals that guide the development of TRM cells, Kupper and his colleagues, led by postdoctoral fellow Youdong Pan, PhD, took an unbiased approach. They measured the level of gene activity for every gene in the genome as the cells developed in mice. That led the team to a remarkable finding, reported in a recent issue of the journal Nature: genes involved in lipid metabolism are highly active in TRM cells, roughly 20- to 30-fold more active than in other types of T-cells. Among these genes are two key mediators of lipid uptake, fatty-acid-binding proteins 4 and 5 (Fabp4 and Fabp5).
Kupper and his colleagues teamed up with Gökhan Hotamisligil, PhD, an expert in lipid biology and metabolism at the Harvard T. H. Chan School of Public Health, to further dissect the roles of Fabp4 and Fabp5 in TRM cells. They found that TRM cells that lack both genes show a striking defect in their ability to import lipids. (Cells lacking just one of the genes are unaffected, likely because the two genes are highly related and perform overlapping functions.) Moreover, these Fabp4- and Fabp5-deficient TRM cells are significantly compromised both in their ability to protect against infection and their long-term survival in peripheral tissues.
Based on his team's recent work, Kupper says the picture that is emerging of TRM cells highlights a unique dependence on fatty acids and other lipids as an energy source. Other types of T-cells can also metabolize lipids, but they cannot take them up from the environment, as TRM cells can. This could become an important Achilles' heel for investigators to target in the future.
Drugs aimed at inhibiting lipid uptake could enable the selective removal of TRM cells from tissues, while leaving other types of T-cells intact. Current therapies for autoimmune disease are fairly broad in their activity—quieting down many types of immune cells, including TRM cells. But they work transiently, likely because TRM cells remain in place.
"I think the real potential pay off of this story is to try and use this new information therapeutically," said Kupper. "While there are treatments for autoimmune diseases that impact pathogenic tissue-resident memory T-cells, none are able to effectively remove the cells from tissues. We've identified the first plausible mechanism for doing just that."
More information: Youdong Pan et al, Survival of tissue-resident memory T cells requires exogenous lipid uptake and metabolism, Nature (2017). DOI: 10.1038/nature21379
















