New method rescues donor organs to save lives
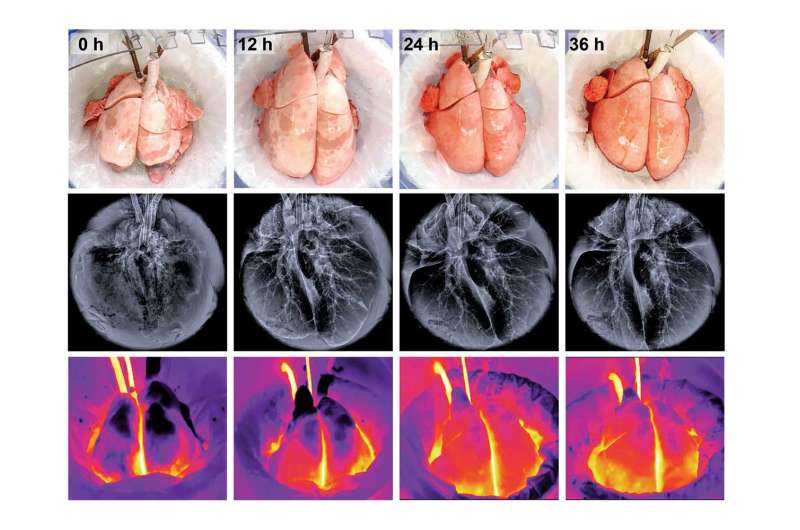
A multidisciplinary team led by Gordana Vunjak-Novakovic, Mikati Foundation Professor of Biomedical Engineering and Medical Sciences at Columbia Engineering, and Matt Bacchetta, associate professor of surgery at Columbia University Medical Center and NewYork-Presbyterian has—for the first time—maintained a fully functional lung outside the body for several days. In a study published today on Nature Biomedical Engineering's website, the researchers describe the cross-circulation platform that maintained the viability and function of the donor lung and the stability of the recipient over 36 to 56 hours. They used the advanced support system to fully recover the functionality of lungs injured by ischemia (restricted blood supply), and made them suitable for transplant.
The team was inspired by the critical need to expand the pool of donor lungs. Transplantation remains the only definitive treatment for patients with end-stage lung disease, but the number of donor lungs is much smaller than the number of patients in need, and many patients die while on the wait list. In addition, lungs quickly lose their function outside the body and during transport: four out of five lungs evaluated at transplant centers are rejected. If these lungs could be kept viable outside the body long enough, it would be possible to improve their function and use them for transplantation.
Over the past five years, Vunjak-Novakovic has been collaborating with Bacchetta and Hans Snoeck, professor of medicine, to investigate how to improve low-quality donor lungs and possibly bioengineer lungs for transplantation. Rather than attempting to build new lungs, they developed strategies to rescue damaged donor lungs. One approach was to use a stem cell therapy of the lung to replace defective cells with new therapeutic cells derived from the transplant recipient. While this technique was applicable to low-quality lungs that are rejected for transplantation, there was a problem: the support of the lung outside the body was too short for the therapeutic cells to start improving lung function.
As often happens, unmet clinical needs inspire new ideas and drive the development of new technologies. The Columbia team realized that "cross circulation"—an abandoned surgical procedure used in the 1960s to exchange blood flow between two patients—could enable long-term support of living organs outside the body by providing critical systemic and metabolic factors that are missing from all current technologies. The team embraced this idea and devised an entirely new approach to support lungs outside the body long enough to enable therapeutic interventions needed to recover their health and normal function.
"This is the most complex study we have ever done, and the one with the highest potential for clinical translation," Vunjak-Novakovic says. "The lung is a masterpiece of 'engineering by nature,' with its more than 40 cell types, and a gas exchange surface area of 100 square meters - half a tennis court. It is amazing that such an intricate organ can be maintained outside the body and even recovered following injury."
"Our team worked hard to innovate a suite of imaging and targeted delivery technologies and ultimately completed this challenging, paradigm-shifting study in less than a year. This was only possible because of our uniquely talented team of bioengineers and surgeons, and the highly collaborative environment at Columbia that fosters innovation," Vunjak-Novakovic says.
The team's breakthrough was realizing that cross-circulation could be re-configured to help recover damaged donor organs. The study's lead authors, PhD candidate John O'Neill and postdoctoral research fellow Brandon Guenthart, looked at clinical studies from the 1960s that used cross-circulation of blood between a healthy individual and a patient suffering from a critical but potentially reversible illness. Working in Vunjak-Novakovic's Laboratory for Stem Cells and Tissue Engineering, they developed a radically new technology to support fully functional lung outside the body for several days.
"Our cross-circulation platform will likely allow us to extend the duration of support to a week or longer if needed, potentially enabling the recovery of severely damaged organs," observes O'Neill. "Beyond prolonging support time, we also demonstrated several therapeutic interventions that vastly improve and accelerate recovery."
As the team was developing their cross-circulation platform, they overcame many challenges to keep the lungs viable outside the body much longer than any platform had before. To prevent the outer surface of the lung from drying out and to provide normal body temperature, they designed a humidification system with ambient temperature control and a re-circulating warm water organ basin to provide normal body temperature to mimic the chest cavity.
Then they needed to tackle the perfusion circuit. To allow for adequate blood flow into and out of the lungs during cross-circulation, they developed new components and techniques and used a donor vessel as a "bio-bridge." They engineered a dynamic system capable of height and hydrostatic pressure adjustments and feedback-regulated pressure-controlled flow. They also developed image-guided techniques for the controlled delivery of drugs and cells in precisely targeted regions of the lung without the need for repeated lung biopsies.
"As our work progressed, we continued to innovate out of necessity and refine and streamline our cross-circulation setup and procedure," says Guenthart.
The researchers say their new platform could be readily extended to recover other organs that are in high demand for transplant or in need of repair, including livers and kidneys, and they have already begun studies in these directions.
"Cross-circulation has proven to be a valuable tool for investigation and has fostered interdisciplinary collaborations," Bacchetta says. "Our study is giving researchers new opportunities to investigate donor-recipient immunologic interactions, therapeutic cell delivery, stem cell differentiation, acute lung injury, and the development of new pulmonary theranostics."
Vunjak-Novakovic adds, "Our goal was to develop a platform that harnesses the full potential of tissue engineering and regenerative medicine toward organ rescue. We hope that our unique technology will benefit the many patients in need and help them live fuller and happier lives."
More information: "Cross-circulation for extracorporeal support and recovery of the lung," Nature Biomedical Engineering(2017). DOI: 10.1038/s41551-017-0037


















