Food insecurity can affect your mental health
Food insecurity (FI) affects nearly 795 million people worldwide. Although a complex phenomenon encompassing food availability, affordability, utilization, and even the social norms that define acceptable ways to acquire food, FI can affect people's health beyond its impact on nutrition. A new study published in the American Journal of Preventive Medicine determined that FI was associated with poorer mental health and specific psychosocial stressors across global regions (149 countries), independent of individuals' socioeconomic status.
Nearly one in three individuals (29.2%) globally experience a common mental disorder during their lifetime, such as depression, anxiety, and somatic symptom disorders. FI may be a key contributor to common mental disorders through several different mechanisms. First, by generating uncertainty over the ability to maintain food supplies or to acquire sufficient food in the future, FI can provoke a stress response that may contribute to anxiety and depression. Furthermore, acquiring foods in socially unacceptable ways can induce feelings of alienation, powerlessness, shame, and guilt that are associated with depression. FI may also magnify socioeconomic disparities within households and communities that could increase cultural sensitivities and influence overall mental well-being.
Andrew D. Jones, PhD, of the Department of Nutritional Sciences, School of Public Health, University of Michigan, Ann Arbor, MI, USA, conducted this research using data from the 2014 Gallup World Poll (GWP). The GWP is a series of nationally representative surveys of individuals 15 years and older that uses probability sampling covering both urban and rural areas. FI data were available for 147,826 individuals across 11 world regions encompassing 149 countries. The extent of FI ranged from 18.3% in East Asia to 76.1% in Sub-Saharan Africa.
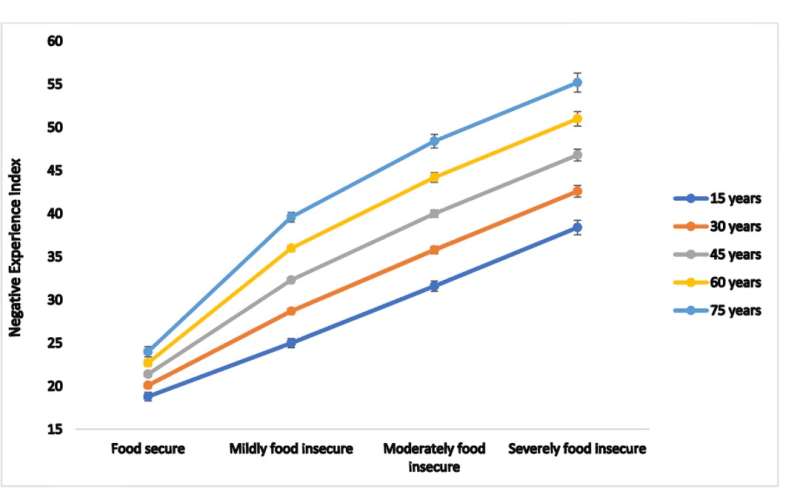
Mental health status was determined using the Negative Experience Index (NEI) and the Positive Experience Index (PEI), two five-question surveys that examine topics such as pain, sadness, enjoyment, feelings of respect, and other factors. Data for the mental health indices were available for 152,696 individuals. The PEI was highest in Latin America and the Caribbean region (79.4) and lowest in Russia and the Caucasus (59.2), while the NEI was lowest in Central Asia (17.4) and highest in the Middle East and North Africa region (34.9).
Dr. Jones found that FI was associated with poorer mental health status in a dose-response fashion, comparing NEI vs. FI for multiple age ranges. An inverse effect was found for PEI vs. FI data.
The consistent dose-response trend suggests a causal association between FI and mental health status. According to Dr. Jones, "This trend suggests that the psychosocial stressors that underlie the mental health indices examined may be amplified with increasing FI. For example, anxiety related to one's ability to acquire sufficient food in the future may be provoked even under conditions of mild FI, and is likely to increase with moderate and severe FI. Alternatively, multiple pathways from FI to poorer mental health may be invoked with increasing severity of FI. Under conditions of more severe FI, for example, individuals may resort to acquiring food in socially unacceptable ways as a coping strategy. The feelings of shame and guilt associated with this behavior could compound pre-existing anxiety precipitated by mild FI to yield even poorer mental health conditions."
Dr. Jones acknowledges the possibility that the direction of the association between FI and mental health status could be the reverse - that poor mental health could drive FI. However, this is the first study to carry out a global analysis of this association and it should inspire further research. Dr. Jones explained, "Developing robust monitoring systems and strengthening the measurement of both FI and mental health to more comprehensively understand their relation across contexts may help to inform interventions that can effectively address the mental health consequences of FI."
More information: Andrew D. Jones, Food Insecurity and Mental Health Status: A Global Analysis of 149 Countries, American Journal of Preventive Medicine (2017). DOI: 10.1016/j.amepre.2017.04.008


















