New study proves one lung cancer subtype can switch to another
A new study co-authored by a researcher starting her laboratory at the University of Kentucky Markey Cancer Center shows that in certain genetic situations, one non-small cell lung cancer subtype can change into another subtype.
This lung cancer 'lineage switching' could underlie resistance to therapeutics, and this research examines exactly how the lineage switch can happen. The work was a collaborative effort between laboratories in Kentucky, New York and Boston.
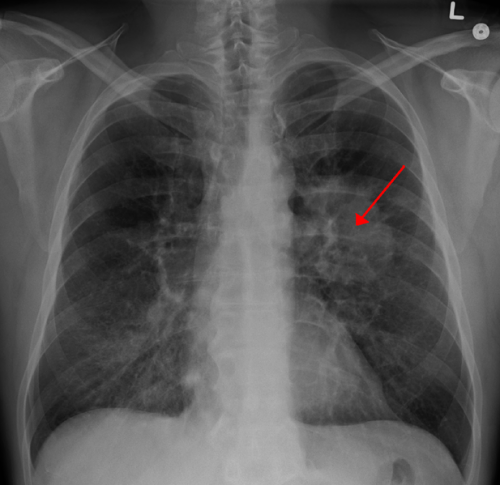
Previously, it was unclear which cells in the adult lung can be the 'cells-of-origin' of the two major subtypes of non-small cell lung cancer, namely adenocarcinoma and squamous cell carcinoma. Likewise, it was unclear what differences in DNA organization define the two distinct lung cancer subtypes. The existence of adenosquamous lung tumors, clinically defined by the presence of both glandular adenocarcinoma lesions and fully stratified squamous lesions within the same tumor, suggested that both adenocarcinomas and squamous cell carcinomas could come from the same cells in the lung, but clear evidence for this theory was lacking.
Published in Nature Communications, the study showed that adenocarcinoma cells can change to squamous cells due to reorganization of their DNA in specific ways. Beginning with a mouse model of adenosquamous lung tumors, researchers validated the genetics by comparing it to human adenosquamous lung tumor – the genetics are often the same, including activation of the oncogene KRAS and the deletion of the tumor suppressor Lkb1. The team then used transplant assays to demonstrate that established adenocarcinoma tumors could transition to squamous cell carcinomas in the mouse lung.
Lastly, the group isolated different lung cells, and demonstrated that only certain lung cells could give rise to tumors capable of undergoing the lineage switch.
"This data is exciting because it shows which cells in the lung can give rise to adenosquamous tumors," said study co-author Christine Fillmore Brainson, assistant professor in the UK department of toxicology and cancer biology. "And the technique we used to transform the isolated cells can be applied to many lung cancer models."
Oncologists have observed this 'lineage switching' after the failure of EGFR tyrosine kinase inhibitor treatment, when it is clinically justifiable to take a second biopsy. However, second biopsies are not normally done after chemotherapy, a practice that Brainson thinks could be revised to understand the exact mechanisms of therapy resistance.
"Now that we have a glimpse into the molecular mechanism of lineage switching, we can begin to learn how to manipulate this phenomenon for better therapeutic outcomes," said Brainson.
More information: Haikuo Zhang et al. Lkb1 inactivation drives lung cancer lineage switching governed by Polycomb Repressive Complex 2, Nature Communications (2017). DOI: 10.1038/ncomms14922














