December 15, 2017 report
Drug found that induces apoptosis in myofibroblasts reducing fibrosis in scleroderma
(Medical Xpress)—An international team of researchers has found that the drug navitoclax can induce apoptosis (self-destruction) in myofibroblasts in mice, reducing the spread of fibrosis in scleroderma. In their paper published in the journal Science, the group describes their study of fibrosis in scleroderma and how they used what they learned to discover the healing effects of navitoclax.
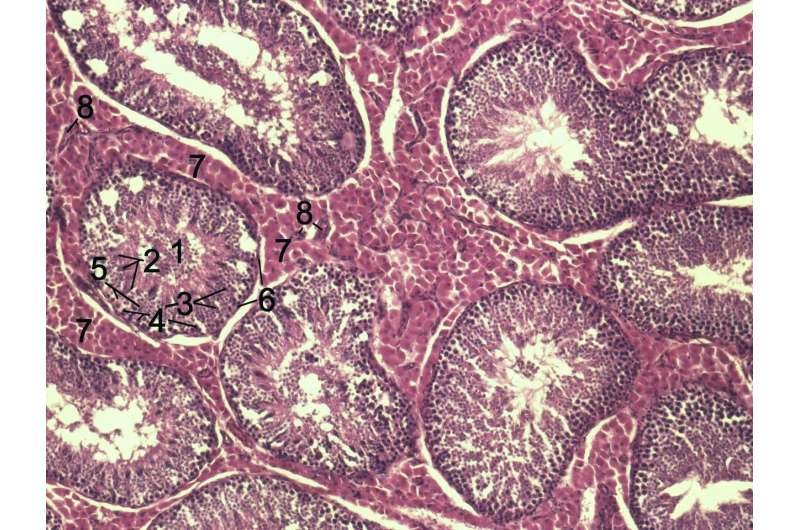
In humans (and mice), fibrosis is seen as a type of scarring that causes damage to organs, sometimes leading to death. Prior research has shown that fibrosis is caused by myofibroblasts, which are cells that are normally involved in helping the body heal. But sometimes, they continue working even after the healing is over, causing scarring. The myofibroblasts continue working, the researchers explain, because they fail to self-destruct as they are supposed to. In this new effort, the researchers sought to learn more about this process by studying one form of fibrosis called scleroderma, which, as its name suggests, starts in the skin before moving to organs.
In taking a closer look at the myofibroblast cell, the researchers found that its mitochondria contained the type of protein normally involved in apoptosis, but the cell did not die—likely, they thought, because it was not being activated. That discovery led them to look at a family of proteins called BCL-2, which either induce or prevent the onset of apoptosis. Further study led to one particular protein called Bcl-xL, which stops apoptosis—they found it in abundance in myofibroblasts. That led them to wonder if there might be a drug that could reduce those levels, thereby allowing the cells to die a proper death. They noted that a drug called ABT-263, more easily remembered as the drug navitoclax, currently undergoing clinical trials as a cancer treatment, also did just what they were looking for.
Testing the drug in mice showed not only that they were on the right track, but that the drug could actually cause the myofibroblasts to die on schedule as they were supposed to, preventing new fibrosis from occurring. But they also noticed something else—the drug appeared to reduce existing fibrosis, as well, though the team could not explain why.
Much more work will have to be done with the drug before it can be considered as a treatment for fibrosis in humans, but at this time, the researchers note, it looks promising.
More information: David Lagares et al. Targeted apoptosis of myofibroblasts with the BH3 mimetic ABT-263 reverses established fibrosis, Science Translational Medicine (2017). DOI: 10.1126/scitranslmed.aal3765
Abstract
Persistent myofibroblast activation distinguishes pathological fibrosis from physiological wound healing, suggesting that therapies selectively inducing myofibroblast apoptosis could prevent progression and potentially reverse established fibrosis in diseases such as scleroderma, a heterogeneous autoimmune disease characterized by multiorgan fibrosis. We demonstrate that fibroblast-to-myofibroblast differentiation driven by matrix stiffness increases the mitochondrial priming (proximity to the apoptotic threshold) of these activated cells. Mitochondria in activated myofibroblasts, but not quiescent fibroblasts, are primed by death signals such as the proapoptotic BH3-only protein BIM, which creates a requirement for tonic expression of the antiapoptotic protein BCL-XL to sequester BIM and ensure myofibroblast survival. Myofibroblasts become particularly susceptible to apoptosis induced by "BH3 mimetic" drugs inhibiting BCL-XL such as ABT-263. ABT-263 displaces BCL-XL binding to BIM, allowing BIM to activate apoptosis on stiffness-primed myofibroblasts. Therapeutic blockade of BCL-XL with ABT-263 (navitoclax) effectively treats established fibrosis in a mouse model of scleroderma dermal fibrosis by inducing myofibroblast apoptosis. Using a BH3 profiling assay to assess mitochondrial priming in dermal fibroblasts derived from patients with scleroderma, we demonstrate that the extent of apoptosis induced by BH3 mimetic drugs correlates with the extent of their mitochondrial priming, indicating that BH3 profiling could predict apoptotic responses of fibroblasts to BH3 mimetic drugs in patients with scleroderma. Together, our findings elucidate the potential efficacy of targeting myofibroblast antiapoptotic proteins with BH3 mimetic drugs in scleroderma and other fibrotic diseases.
© 2017 Medical Xpress


















