Overlooked immune cells hold breakthrough for treating aggressive cancers
The latest generation of cancer treatments spring from the discovery that the human immune system is able to beat the disease. Like Dorothy in "The Wizard of Oz," what research teams around the world have spent decades searching for was right in their own backyard all along.
Adoptive cell transfer, or ACT, is one of these new immune-based treatments. For ACT, doctors draw a sample of blood from a cancer patient, sift out naturally occurring immune system T cells and re-engineer them in a laboratory, turning them into super-charged, cancer fighters. Then, billions of these killer T cells are put back into the patient's bloodstream, where they hunt down and destroy the cancer.
ACT is now one of the most effective treatments for melanoma and many blood-based cancers. Unfortunately, it is not very effective against aggressive solid tumors, such as pancreatic cancer. The problem is there are hundreds of types of T cells in the body, and not all of them make good cancer fighters. It is very difficult to identify and sift out the exact T cells needed to fight highly malignant tumors. The T cells must be able to both navigate their way to the tumor and survive long enough in the harsh cancer environment to kill all of the cancer.
Luckily, identifying these resilient, cancer-killing T cells just got a lot easier, thanks to a team of Hollings Cancer Center researchers at the Medical University of South Carolina (MUSC), led by Chrystal Paulos, Ph.D., associate professor of Microbiology and Immunology and the Cecilia and Vincent Peng Endowed Chair in Melanoma and Cutaneous Oncology. Their breakthrough discovery, published in the December 2017 issue of Nature Communications, finds that T cells with a protein called CD26 on their surface have the best cancer-fighting potential.
The road to this discovery began when the team started looking at a group of T cells that are not widely used for ACT. There are many different T cell 'families,' and most ACT treatments use T cells from the CD8 family. But the Paulos team chose to focus on the CD4 family.
Stefanie Bailey, a graduate student on Paulos' team and lead author on the article, explains. "CD4 T cells get overlooked in cancer immunotherapy. There's a bias in the field to study CD8 T cells, because they're known to have strong anti-cancer abilities," she says. "CD4 T cells are mostly known for helping other cells function—in fact, CD4 T cells are called 'T-helper cells.' But studies show that CD4 T cells can also clear cancer."
Last spring, the team discovered that a particular type of CD4 T cells, called Th17 cells, were highly effective against aggressive solid tumors. But they needed a way to identify Th17 cells in a blood sample, so they could sift them out and use them for ACT therapy. Then, a new study caught Bailey's attention. It showed that T cells with a protein called CD26 on their surface carried markers for Th17.
"We were looking for a way to get Th17 cells directly from patients' blood to get around having to generate them in the lab, which is a very complex process," says Bailey. "We needed a simple way to identify Th17 cells. So, when we saw that Th17 cells express high levels of CD26, we wanted to explore it. CD26 is a multi-functional protein that's on the surface of the cell. It's actually pretty well-known in the immunology field."
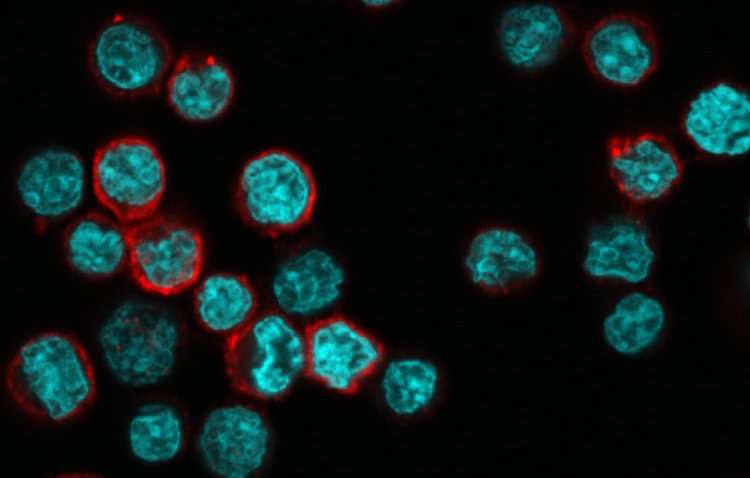
Although CD26 was well known, Paulos' team was the first to study its role in fighting cancer. The first thing they found was that all CD4 T cells did not have the same amount of CD26 on the surface. Some had little or no CD26, some had intermediate levels and others had high CD26. In addition, these three T cell groups had very different abilities to fight cancer.

The team expected T cells with high CD26 levels to perform worst against cancer, because initial tests showed that high-CD26 T cells had many hallmarks of being weak immune cells. To their surprise, closer study showed quite the opposite.
"We were really shocked to see that these cells could not only kill multiple solid tumors but also could survive for a long time in the patient," says Bailey. "When you look at high-CD26 T cells, they look exhausted. They appear incapable of mounting a long-term response to cancer. They don't look at all like the kind of T cells we would want for therapy," she explains.
Despite their appearance, high-CD26 T cells had two critical characteristics the other two types lacked. First, they could resist apoptosis (processes that lead to cell death) and survive in the hostile tumor environment. Second, they had stem cell-like properties, allowing them to repopulate and keep growing after being infused into the patient.
"One of the beauties of ACT is that it's a living therapy," says Bailey. "After the T cells kill the tumor, they keep living inside the patient. So, if the tumor comes back, you already have T cells there that can kill it again." Theoretically, ACT-infused T cells can last a lifetime. Viable, re-infused T cells have been found over twenty years later in ACT patients.
The team's discovery that T cells with high levels of CD26 are excellent cancer fighters will help advance the use of T cell-based immunotherapies for cancer and other autoimmune diseases. Until now, researchers looked for multiple markers to identify the best T cells for ACT. This breakthrough suggests that the long list of markers can be shortened to just one: CD26.
"There are two really exciting things here," says Bailey. "First, you can identify T cells with superior therapeutic potential by how much CD26 they have. So, you can maximize the chance that ACT will succeed in killing the cancer. Second, in the solid tumors we looked at, having T cells with CD26 at the tumor site produced a better therapeutic response, suggesting that having CD26 expression on tumor-infiltrating T cells directly correlates with the patient's response."
The study specifically looked at melanoma, mesothelioma and pancreatic cancer. Animal models bearing these types of tumors experienced a better treatment outcome when a heightened percentage of CD26 donor T cells infiltrated the tumor. There was a 50 percent curative rate in melanoma and 95 percent for mesothelioma. There was not a curative response for pancreatic cancer, but it did reduce tumor size by two-thirds and extend survival in the preclinical model. These findings suggest that it may work well in combination therapies, she says.
"We're excited about the broader clinical implications of this discovery," adds Paulos. "Targeting T cells with CD26 will not only benefit ACT therapy but will also help bolster the effectiveness of other cancer immunotherapies, such as checkpoint modulators, vaccines and cytokine therapies." Paulos explained that human CD4 T cells expressing various amounts of CD26 could also be manipulated in treating patients with infectious diseases and autoimmune manifestations.
Now the Paulos laboratory is collaborating with investigators at MUSC and around the world to further explore the role of CD4 T cells with different CD26 levels in different types of cancer and autoimmune diseases. Beyond providing more effective treatments, it also offers other benefits. "If you get the right types of cells, maybe you don't need as many. It could cut down on a lot of expenses and the time patients would need to get the treatment" says Paulos.
More information: Stefanie R. Bailey et al, Human CD26high T cells elicit tumor immunity against multiple malignancies via enhanced migration and persistence, Nature Communications (2017). DOI: 10.1038/s41467-017-01867-9
















