Personalized blood sugar goals can save diabetes patients thousands
A cost analysis by researchers at the University of Chicago Medicine shows treatment plans that set individualized blood sugar goals for diabetes patients, tailored to their age and health history, can save $13,546 in health care costs over their average lifetime when compared with treatment strategies that stick to a uniform national standard.
The study, published December 12 in the Annals of Internal Medicine, showed the majority of those savings come from lower medication costs. Individualized care also slightly increased quality-adjusted life years, or the amount of time spent living in relative good health without severe complications.
"People don't want to be treated by a standard value or an algorithm, they want to be treated like individuals," said Neda Laiteerapong, MD, assistant professor of medicine at UChicago Medicine and lead author of the study.
"I think this model will give evidence to physicians that individualized glycemic control is something to consider. It can help save our health system money, and it's in line with what many patients want," she said.
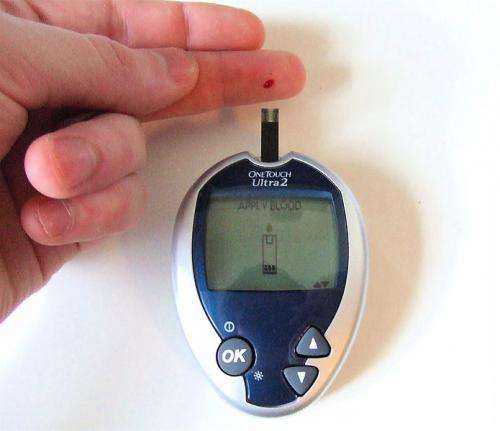
Hemoglobin A1C is a common measure of blood sugar control for diabetics, measured as a percentage of blood cells that carry extra glucose molecules. The lower the A1C percentage, the better, and for years the American Diabetes Association (ADA) recommended a standard goal of less than seven percent for most diabetics.
In 2012, the ADA and the European Association for the Study of Diabetes published a statement recommending that physicians individualize blood sugar goals based on several factors, including age, life expectancy, complications and how long a patient has had diabetes. In many cases, say for an elderly patient who has been living with diabetes for decades and has several complications, aggressive blood sugar control may not be appropriate, so they can set a higher A1C target of less than eight percent.
In the new study, Laiteerapong and her colleagues used a statistical model that calculated health care costs over the average expected lifetime of the patients, using data from 569 patients in the National Health and Nutrition Examination Survey (NHANES) who are representative of the population of U.S. adults over the age of 30 with type 2 diabetes. The model factored in variables such as age, duration of diabetes and history of complications such as heart disease, hypertension, stroke, retinopathy and kidney disease. It assigned costs for typical type 2 diabetes treatment regimens with drugs like metformin, insulin and sulfonylureas, and included standard values from the research literature for the cost of treating major events like a heart attack or stroke.
Using this input data, they ran 2,500 simulations for the expected remaining lifetime of each patient with both treatment strategies: a personalized A1C value which changed over their lifetime, versus a standard, uniform value less than seven. The model showed that the individualized control strategy saved on average $13,564 per person compared to the uniform strategy ($105,307 vs. $118,853 lifetime). The difference was almost entirely due to lower medication costs ($34,521 vs. $48,763). Given that roughly 17.3 million adults in the U.S. over 30 have type 2 diabetes, this could amount to a whopping $234 billion lifetime savings nationwide.
The model did predict a slight decrease in life expectancy (36 days) due to an increase in complications on the personalized strategy. Laiteerapong attributes that to statistical limitations in the model that don't account for long-term, cumulative benefits of treatment.
"The differences in life expectancy and complication rates were very small, but choosing a personalized A1C goal can reduce medications by half per year," Laiteerapong said. "If I told my patients they could take half as many medications but maybe there's a small chance they might live a month less, I'm pretty sure many of them would sign up for it."
More information: "Cost-effectiveness Analysis of Individualized Glycemic Control for U.S. Adults with Type 2 Diabetes," Annals of Internal Medicine (2017). DOI: 10.7326/M17-0537



















