New biomarkers predict outcome of cancer immunotherapy
Researchers at the University of Zurich have identified biomarkers in the blood that make it possible to predict whether cancer patients will respond positively to immunotherapy. Pa-tients for whom therapy does not work can thus be treated using different methods at an earlier stage.
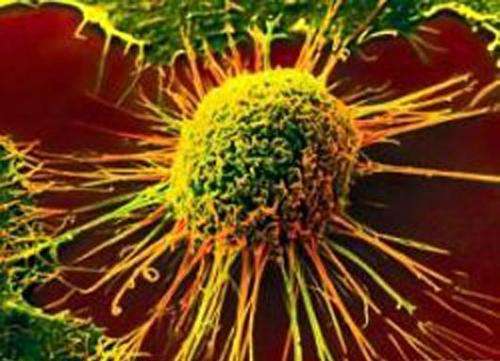
Nowadays, melanoma and lung cancer can be combatted effectively through immunotherapy, which makes targeted use of the immune system's normal function of regularly examining the body's tissue for pathogens and damages. Specific inhibitors are used to activate immune cells in a way that makes them identify cancer cells as foreign bodies and eliminate them. This way, the immune system can boost its often weak immune response to allow it to even detect and destroy metastatic cancer cells. Immunotherapy thus makes it possible to control cancer cells in up to 50 percent of patients, in some cases even curing them altogether.
Not all respond to immunotherapy
However, around half of cancer patients do not respond to immunotherapy, but still have to put up with its side effects. A team of researchers from the University of Zurich and the UniversityHos-pital Zurich has now used a novel method to find out which patients are likely to respond positive-ly to immunotherapy. The researchers were able to identify biomarkers in the blood that indicate whether the therapy is highly likely to be effective even before treatment is commenced.
"The blood counts of patients should be analyzed for these biomarkers when making a decision about immunotherapy. This will dramatically increase the share of patients who will benefit from this type of therapy," says Professor Burkhard Becher from the Institute of Experimental Immunol-ogy at UZH. "At the same time, it makes it possible to directly move on to different methods in cases where immunotherapy won't work - without losing valuable time."
High-dimensional cell analysis
The researchers worked hand in hand with the Department of Dermatology of the UniversityHospi-tal Zurich to examine biomarkers in 40 blood samples of 20 patients, both before and 12 weeks after immunotherapy. For this, they used the high-dimensional "cytometry by time of flight" (Cy-TOF) cell analysis method, which analyzes cells for up to 50 different proteins one cell at a time. The researchers were thus able to differentiate every single cell and document its activation sta-tus. Even nuanced differences between the patient samples were recorded in detail.
Recognizing molecular patterns
After analyzing the cells, the researchers examined the data together with employees of the Swiss Institute of Bioinformatics at UZH in terms of molecular patterns that could predict therapeu-tic success. "Even before the start of a therapy, we observed a subtle and weak immune re-sponse in the blood, and identified this molecular pattern as the immune cells CD14+CD16−HLA-DRhi," says Burkhard Becher. For the finding to be easily verifiable, the biomarkers should be easi-ly detectable; indeed, the blood count was able to be validated using conventional methods in a second, independent cohort of more than 30 people.
Dawning of precision medicine
"Together with comprehensive, precisely structured biobanking, this study represents a major step towards precision medicine," says Professor Mitch Levesque of the Department of Dermatology at the UniversityHospital Zurich. Before they can be used clinically, the insights gained must now be applied in independent studies with higher patient numbers. The method using biobanking, high-dimensional cytometry, and computer-aided pattern recognition should also be useful in clinical decision support and developing new therapeutic approaches when it comes to other clinical pictures.
More information: Carsten Krieg, Malgorzata Nowicka, Silvia Guglietta, Sabrina Schindler, Felix J Hartmann, Lukas M Weber, Reinhard Dummer, Mark D Robinson, Mitchell P Levesque & Burkhard Becher. High-dimensional single-cell analysis predicts response to anti-PD-1 immunotherapy. Nature Medicine, 8 January 2018. DOI: 10.1038/nm.4466














