Gene therapy restores normal blood glucose levels in mice with type 1 diabetes
Type 1 diabetes is a chronic disease in which the immune system attacks and destroys insulin-producing beta cells in the pancreas, resulting in high blood levels of glucose. A study published January 4th in Cell Stem Cell demonstrates that a gene therapy approach can lead to the long-term survival of functional beta cells as well as normal blood glucose levels for an extended period of time in mice with diabetes. The researchers used an adeno-associated viral (AAV) vector to deliver to the mouse pancreas two proteins, Pdx1 and MafA, which reprogrammed plentiful alpha cells into functional, insulin-producing beta cells.
"This study is essentially the first description of a clinically translatable, simple single intervention in autoimmune diabetes that leads to normal blood sugars, and importantly with no immunosuppression," says senior study author George Gittes of the University of Pittsburgh School of Medicine. "A clinical trial in both type 1 and type 2 diabetics in the immediate foreseeable future is quite realistic, given the impressive nature of the reversal of the diabetes, along with the feasibility in patients to do AAV gene therapy."
Approximately 9% of the world's adult population has diabetes, which can cause serious health problems such as heart disease, nerve damage, eye problems, and kidney disease. One fundamental goal of diabetes treatment is to preserve and restore functional beta cells, thereby replenishing levels of a hormone called insulin, which moves blood glucose into cells to fuel their energy needs. But in patients with type 1 diabetes, beta-cell replacement therapy is likely doomed to failure because the new cells might fall victim to the same autoimmunity that destroyed the original cells.
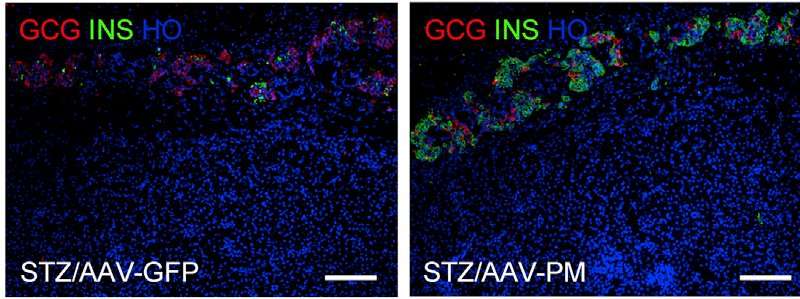
A potential solution to this problem is to reprogram other cell types into functional beta-like cells, which can produce insulin but are distinct from beta cells and therefore are not recognized or attacked by the immune system. To explore the feasibility of this approach, Gittes and first author Xiangwei Xiao of the University of Pittsburgh School of Medicine engineered an AAV vector to deliver to the mouse pancreas proteins called Pdx1 and MafA, which support beta cell maturation, proliferation, and function. The goal was to generate functional beta-like cells from pancreatic alpha cells, which may be the ideal source for beta cell replacement. For example, alpha cells are plentiful, resemble beta cells, and are in the correct location, all of which could facilitate reprogramming.
By comparing the gene expression patterns of normal beta cells and insulin-producing cells derived from alpha cells, the researchers confirmed nearly complete cellular reprogramming. This gene therapy approach restored normal blood glucose levels in diabetic mice for an extended period of time, typically around four months, and the new insulin-producing cells derived almost exclusively from alpha cells. Moreover, the strategy successfully generated functional insulin-producing cells from human alpha cells.
"The viral gene therapy appears to create these new insulin-producing cells that are relatively resistant to an autoimmune attack," Gittes says. "This resistance appears to be due to the fact that these new cells are slightly different from normal insulin cells, but not so different that they do not function well."
Several features of this approach could facilitate translation to humans. For one, AAV vectors like those used in this study are currently undergoing various gene therapy trials in humans. Moreover, the viral vectors can be delivered directly to the human pancreas through a routinely performed non-surgical endoscopic procedure; however, this procedure can elicit pancreatic inflammation. In addition, no immunosuppression is required, so patients would avoid related side effects such as an increased risk of infection.
However, one major concern was that the mice did eventually return to the diabetic state, suggesting that this treatment would not represent a definitive cure for the disease. "The protection from recurrent diabetes in the mice was not permanent, although some studies would suggest that processes in mice are highly accelerated, so four months in mice might translate to several years in humans," Gittes says.
Currently, the researchers are testing their approach in primates. "If we are able to show efficacy in non-human primates, we will begin work with the FDA to get approval for the use of this viral gene therapy in diabetic patients, both type 1 and type 2," Gittes says.
More information: Cell Stem Cell, Xiao et al.: "Endogenous Reprogramming of Alpha Cells into Beta Cells, Induced by Viral Gene Therapy, Reverses Autoimmune Diabetes" www.cell.com/cell-stem-cell/fu … 1934-5909(17)30472-1 , DOI: 10.1016/j.stem.2017.11.020

















