Brain cholesterol associated with increased risk of Alzheimer's disease
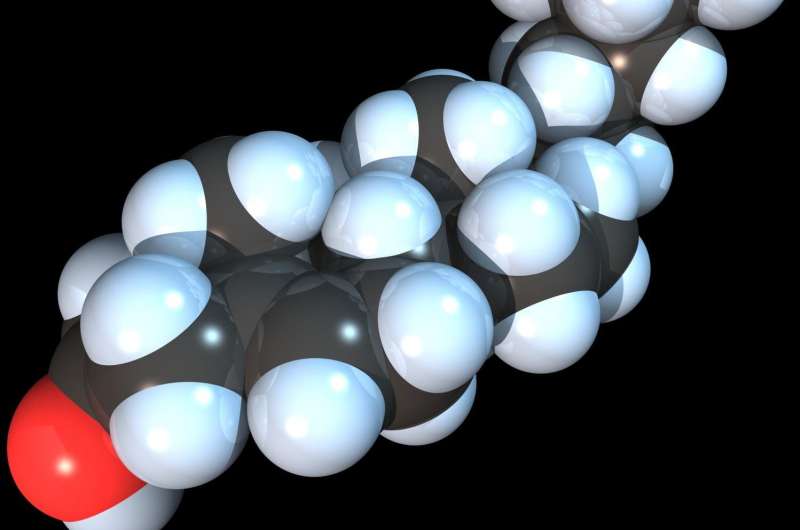
Researchers have shown how cholesterol—a molecule normally linked with cardiovascular diseases—may also play an important role in the onset and progression of Alzheimer's disease.
The international team, led by the University of Cambridge, have found that in the brain, cholesterol acts as a catalyst which triggers the formation of the toxic clusters of the amyloid-beta protein, which is a central player in the development of Alzheimer's disease.
The results, published in the journal Nature Chemistry, represent another step towards a possible treatment for Alzheimer's disease, which affects millions worldwide. The study's identification of a new pathway in the brain where amyloid-beta sticks together, or aggregates, could represent a new target for potential therapeutics.
It is unclear if the results have any implications for dietary cholesterol, as cholesterol does not cross the blood-brain barrier. Other studies have also found an association between cholesterol and the condition, since some genes which process cholesterol in the brain have been associated with Alzheimer's disease, but the mechanism behind this link is not known.
The Cambridge researchers found that cholesterol, which is one of the main components of cell walls in neurons, can trigger amyloid-beta molecules to aggregate. The aggregation of amyloid-beta eventually leads to the formation of amyloid plaques, in a toxic chain reaction that leads to the death of brain cells.
While the link between amyloid-beta and Alzheimer's disease is well-established, what has baffled researchers to date is how amyloid-beta starts to aggregate in the brain, as it is typically present at very low levels.
"The levels of amyloid-beta normally found in the brain are about a thousand times lower than we require to observe it aggregating in the laboratory—so what happens in the brain to make it aggregate?" said Professor Michele Vendruscolo of Cambridge's Centre for Misfolding Diseases, who led the research.
Using a kinetic approach developed over the last decade by the Cambridge team and their collaborators at Lund University in Sweden, the researchers found in in vitro studies that the presence of cholesterol in cell membranes can act as a trigger for the aggregation of amyloid-beta.
Since amyloid-beta is normally present in such small quantities in the brain, the molecules don't normally find each other and stick together. Amyloid-beta does attach itself to lipid molecules, however, which are sticky and insoluble. In the case of Alzheimer's disease, the amyloid-beta molecules stick to the lipid cell membranes that contain cholesterol. Once stuck close together on these cell membranes, the amyloid-beta molecules have a greater chance to come into contact with each other and start to aggregate—in fact, the researchers found that cholesterol speeds up the aggregation of amyloid-beta by a factor of 20.
So what, if anything, can be done to control cholesterol in the brain? According to Vendruscolo, it's not cholesterol itself that is the problem. "The question for us now is not how to eliminate cholesterol from the brain, but about how to control cholesterol's role in Alzheimer's disease through the regulation of its interaction with amyloid-beta," he said. "We're not saying that cholesterol is the only trigger for the aggregation process, but it's certainly one of them."
Since it is insoluble, while travelling towards its destination in lipid membranes, cholesterol is never left around by itself, either in the blood or the brain: it has to be carried around by certain dedicated proteins, such as ApoE, a mutation of which has already been identified as a major risk factor for Alzheimer's disease. As we age, these protein carriers, as well as other proteins that control the balance, or homeostasis, of cholesterol in the brain become less effective. In turn, the homeostasis of amyloid-beta and hundreds of other proteins in the brain is broken. By targeting the newly-identified link between amyloid-beta and cholesterol, it could be possible to design therapeutics which maintain cholesterol homeostasis, and consequently amyloid-beta homeostasis, in the brain.
"This work has helped us narrow down a specific question in the field of Alzheimer's research," said Vendruscolo. "We now need to understand in more detail how the balance of cholesterol is maintained in the brain in order to find ways to inactivate a trigger of amyloid-beta aggregation."
More information: Johnny Habchi et al, Cholesterol catalyses Aβ42 aggregation through a heterogeneous nucleation pathway in the presence of lipid membranes, Nature Chemistry (2018). DOI: 10.1038/s41557-018-0031-x



















